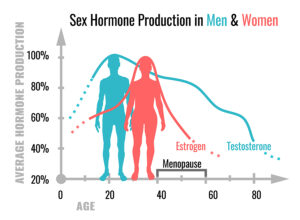
I am describing here that hormones play an important role in survival from Covid-19. There are two publications that illustrate that point.
Estrogens protect women against Covid-19
A study from Dec. 4, 2020 covering 17 countries and involving nearly 70,000 women discovered these principal findings.
- Women aged 20 to 50 have moderately higher Covid-19 infection rates than men
- In all of the age groups men have higher mortality rates than women
- Beyond the age of 50 the fatality rate from Covid-19 is 50% higher in men than that of women
- Postmenopausal women above the age of 50 and on estradiol supplementation had 50% less mortality from Covid-19 than women without estradiol supplementation
The researchers said about the study: “In a nutshell, it’s likely that the apparently protective effects of 17β-estradiol, a naturally occurring, abundant female hormone, relate to a key property of this molecule: it attenuates the so-called “cytokine storm” that’s thought to underlie much of the cellular-scale and organ/tissue-level damage wrought by a SARS-CoV-2 infection, via dysregulation of a patient’s immune response.”
Men need enough testosterone to fight Covid-19
Another study from September 17, 2020 pointed out that males have much worse outcomes with Covid-19 than females. Men are affected by Covid-19 twice as often as females and they experience a much more severe course with a higher mortality. The authors also point out that there is a direct correlation between lower serum testosterone levels in men and inflammation severity by cytokines and poor clinical outcomes. The decline in total and free testosterone in aging men leads to serious pulmonary complications and the need to treat the patient in the ICU. The Covid-19 coronavirus utilizes Angiotensin-Converting Enzyme II (ACE2) for entry into the host cell. A male requires testosterone for ACE2 expression. Lower testosterone causes higher mortality in men. In contrast, if testosterone in a male is too high, blood clots can form in the circulatory system, which often lead to complications and deaths in patients with Covid-19.
Vitamin D levels and course of Covid-19
There are three major effects that vitamin D has.
- A strengthening of the epithelial barrier not allowing the coronavirus to penetrate into the lung tissue as easily.
- Release of defensins and cathelicidin, two crucial antiviral polypeptides, that eradicate the SARS-CoV-2 virus in the system.
- Interruption of the “cytokine storm”, an overwhelming inflammation which is responsible for viral pneumonia to develop. Without the cytokine storm there is no damage to the lungs, and people do not need treatment in the ICU. This is particularly important for people above the age of 60 and for people with pre-existing diseases.
Similarly, with the stabilizing effect of vitamin D regarding the immune function more severe forms of Covid-19 can turn into less severe forms with a better outcome.
Discussion
Research showed that in women estrogen has a modifying effect on the course of Covid-19. In males it is testosterone that leads to an improved course of Covid-19. Both sexes require adequate doses of vitamin D, which helps to strengthen the epithelial barrier. In addition, enough vitamin D releases defensins and cathelicidin, two crucial antiviral polypeptides that eradicate any virus in the system. Vitamin D also interrupts the “cytokine storm”, an overwhelming inflammation, which is responsible for viral pneumonia to develop. All of these factors together modify the course of Covid-19 and improve the probability of survival from this otherwise serious viral illness.
Conclusion
Two lines of research showed that both women and men do better with Covid-19 when their hormone levels are either adequate or are substituted to normal levels. Women in menopause taking estradiol for postmenopausal symptoms had 50% less mortality from Covid-19. Men who were testosterone deficient and were put on testosterone supplementation do better with respect to Covid-19. In aging men total and free testosterone decline and serious pulmonary complications occur with a need to treat the patient in the ICU. On top of hormones both men and women benefit from high doses of vitamin D, which strengthens the epithelial barrier. Vitamin D also releases defensins and cathelicidin, two crucial antiviral polypeptides that fights the SARS-CoV-2 virus directly. In addition, vitamin D interrupts the “cytokine storm”, an overwhelming inflammation which causes the viral pneumonia. Taken together the hormones and vitamin D can improve the outcome of Covid-19 significantly.
This text includes part of this blog.