Dr. Prabhat Jha of the Centre for Global Health Research, Toronto has published research regarding the risk of mortality associated withs smoking in India, involving data from 1.1 million Indian homes. Data of deceased individuals, all of them in the age group between 30 and 69 years of age, showed that 37% of the men and 5% of the women had been smokers, and smoking doubled the risk for both sexes due to medical causes. Smoking did not only rate as a risk for lung and respiratory cancers but also for tuberculosis, vascular and respiratory disease. Smoking as a causal relationship was estimated to be responsible for 1 in 5 deaths in men and 1 in 20 deaths in women. With the population growth in India the number of death in the age group of 30 to 69 related to smoking is estimated to increase by 3% per year. Currently available data suggests that the rate of smoking is high especially among men in India. Data from other nations show, that smoking bans in public places are effective in turning these statistics around. Italy used to be one of the European nations, where smoking in public was common and as a result the exposure to second hand cigarette smoke was not only an inconvenience but a serious health risk. Cardiovascular events like heart attacks showed a decrease among men and women in Italy after the smoking ban in public places was put into effect in 2005. The findings were related to the improved indoor air quality.
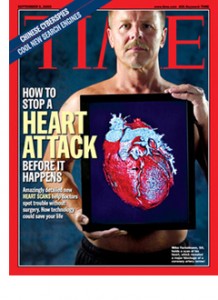
There was an increase of sales in stop smoking aids like nicotine replacement products. Sales of cigarettes showed a decrease. Giulia Cesaroni from a local health unit in Rome remarked that even a small reduction in the incidence of cardiovascular disease can have enormous public health implications, as coronary artery disease is the leading cause of deaths in Italy. Compared to before the ban heart attack rates of middle aged (35- to 64-years) Italians dropped by 11%, 65- to 74-year-olds had a reduction of 8%, but those in the 75-84 year age group showed no benefit (as coronary artery disease in them likely was irreversible).
More information about:
1. Chronic obstructive pulmonary disease: http://nethealthbook.com/lung-disease/chronic-obstructive-pulmonary-disease-copd/
2. Causes of lung cancer: http://nethealthbook.com/cancer-overview/lung-cancer/causes-lung-cancer/
3. Heart attacks: http://nethealthbook.com/cardiovascular-disease/heart-disease/heart-attack-myocardial-infarction-or-mi/
References: The Indian data based on www.nejm.org (February 13, 2008); the Italian study was published in Circulation 2008 (Feb. 11)
Last edited November 3, 2014