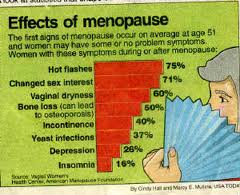
Hormone Replacement Therapy (HRT) has not only benefits. The potential side effects have become evident, and as a result, doctors have cautioned their patients, that HRT may not be the answer for every menopausal woman. However, lately natural hormone replacement therapy has become popular as an alternative. According to statistics only 20% of Asian women are plagued by hot flashes during menopause as compared to 80% of Westerners. A lifestyle intervention trial from Australia taught 120 women to adapt Japanese diet and lifestyle habits. The participants of the trial also started an exercise program for women, drank lots of water, increased calcium intake and increased the intake of plant-estrogens. Researchers had chosen this model, as Japanese women average five more years of healthy living than their sisters in the West. The spotlight of the research continues to focus on plant-based estrogens. Isoflavone precursors are found in soy (which is widely consumed in Asia), but it is also present in fruits, vegetables, legumes and seeds such as flax. We do not know too much about the long-term effect of manufactured or isolated soy products, and so it is best to stay with the natural soy foods such as edamame (soy beans), tofu, tempeh and miso. Beside soy foods, lots of vegetables, beans and fruit are beneficial, and ground flax seed has also shown to decrease menopausal symptoms. Research in Chinese women has shown a modest association between post-menopausal soy intake and increased bone density.
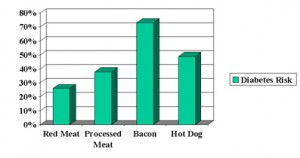
Compared to this, the “typical” North American diet isn’t an accessory to good health; being high in white flour, sugar, trans fat and providing saturated fat of meat and dairy products this is also bad news for menopause. In addition there is a correlation between an increased body mass index and one to five alcoholic drinks per week with increased hot flashes in peri-menopausal women. Research from Simmons College at the Harvard School of Public Health has shown that Western food habits of red meat and processed meats (hot dogs, bacon) put especially women’s health at risk.
| Diabetes Risk Increased With Western Diet Over 14 Years (modified from Archives of Internal Medicine) |
Some experts say that the health of Asian women is more robust due to their life-long soy intake, in which case it would make sense to not even wait for all the dreaded symptoms of menopause to appear, but make way for healthy diet choices early. Soy products have become immensely popular and are readily available in today’s market, and so it will be interesting to see if the next generation of women has an easier time going through menopause.
More info on menopause: http://nethealthbook.com/hormones/hypogonadism/secondary-hypogonadism/menopause/
References: 1.The Medical Post January 25, 2005, page 17 2. The Medical Post, February 1, 2005, page 17
Last edited October 27, 2014