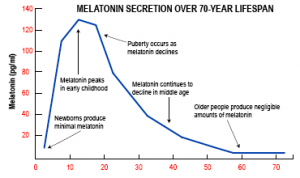
Notably, the January 2021 issue of the Life Extension magazine informs you that melatonin is more than a sleeping aid. It contains an interview between Dr. Roman Rozencwaig and a Life Extension (LE) magazine reporter. It must be remembered that Dr. Rozencwaig dedicated much of his career to the healing effects of melatonin. Another keypoint is that in 1987 Dr. Rozencwaig published a paper together with two other researchers. Specifically, it showed that melatonin production by the pineal gland declines in older age. Markedly, they stated that this is the reason why people age and why diseases of aging develop. Another key point is that Dr. Rozencwaig also stated that taking oral melatonin can promote a healthier life.
Melatonin deficiency causing aging and various illnesses
With the aging process the pineal gland calcifies and melatonin production is steadily declining. Surely, along with this is a deterioration of the circadian hormone rhythm. Meanwhile, the neuroendocrine system in the brain gets disorganized. Accordingly, this causes various diseases to occur. To emphasize, Dr. Rozencwaig says that a proper balance between melatonin and neurotransmitters is what we need to maintain health and longevity. As a result, a daily intake of melatonin supports healthy aging and longevity.
The many clinical effects of melatonin
Oral melatonin tablets help you to fall asleep easier, particularly the population that is older than 60 years.
But besides that, melatonin has many other clinical effects.
- Melatonin improves immunity, which improves resistance against infections. It helps also in cancer prevention
- Melatonin maintains the circadian hormone rhythm by synchronizing pituitary and hypothalamic hormone production
- It protects the brain and may prevent Parkinson’s disease, Alzheimer’s disease, multiple sclerosis, autism, and others
- Melatonin modulates anti-inflammatory cytokinins in different diseases
Dr. Rozencwaig mentioned that melatonin slows down the aging process. There are multiple intertwining reasons for this.
Melatonin’s actions against the aging process
- Melatonin regulates gene expression. This means that some signs and symptoms of aging can be reversed through genetic switches
- Because melatonin regulates the immune response, the body is more protected against viral, bacterial and parasitic infections
- Melatonin helps to overcome chronic inflammation that produces cytokines
- Melatonin is also liver-protective through stimulation of an enzyme (AMPK). This enzyme regulates cellular metabolism.
- There are other processes that melatonin is involved in: energy metabolism by protection and restoration of mitochondria.
- Melatonin protects against osteoporosis by balancing and regulating bone formation versus bone loss.
More actions of melatonin
- An important function of melatonin is the stimulation of antioxidant enzymes like glutathione peroxidase and superoxide dismutase (SOD)
- Melatonin regulates sirtuins, which are proteins that maintain cellular health. They protect you from obesity, type 2 diabetes, cancer, heart attacks and strokes, dementia and more
- As already mentioned, melatonin is a neuroprotective agent and may prevent Alzheimer’s and dementia
- Melatonin stimulates apoptosis of cancer cells.
- Oral health and melatonin are related. Melatonin suppresses herpes infections and periodontal disease. Melatonin prevents oral cancers to a certain degree. In addition, dental implants survive better when melatonin is present in saliva.
Prevention of cognitive decline
Dr. Rozencwaig mentioned that melatonin stops much of the cognitive decline of aging. To achieve this the following processes take place.
- Melatonin improves the sleeping pattern and increases the amount of REM sleep.
- During sleep melatonin removes toxic amyloid and tau proteins. We know that with Alzheimer’s disease these are the proteins that accumulate in the brain.
- Melatonin improves myelination of white matter in the brain. This prevents brain atrophy of old age.
- The brain is metabolically very active and produces toxic free radicals. But melatonin is a strong antioxidant dealing with free radicals. Melatonin can cross the blood brain barrier and stimulates enzyme production to eliminate toxic reactive oxygen species.
- Chronic inflammation also increases with age, but melatonin deals with this condition in the brain.
- Here are 3 subtypes of melatonin receptors. The body integrates the multitude of actions of melatonin with the help of these receptors.
Conclusion
Melatonin is a powerful antioxidant that has many other useful protective qualities as explained. The body integrates various functions like anti-aging, anti-free radical activity, neuroprotection in the brain and more. Melatonin even synchronizes pituitary and hypothalamic hormone production. This helps to integrate the effect of melatonin, which benefits the body in many ways. Melatonin prevents Parkinson’s and Alzheimer’s disease, multiple sclerosis, autism, obesity, type 2 diabetes, cancer, heart attacks, strokes and dementia. Melatonin production deteriorates from the age of about 60 onwards. It is important to supplement with melatonin at nighttime from that age on. Usually, you only need small amounts of melatonin, between 1mg and 3 mg at bedtime. This prevents most of the serious diseases of old age, stimulates your immune system and lets you age gracefully.