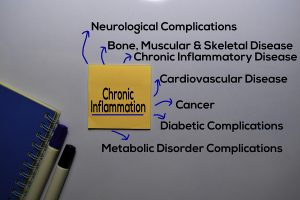
A CNN review article noted that anti-inflammatory diets improve inflammation. This is important for medical conditions that also have inflammation attached to it. For instance, rheumatoid arthritis, diabetes or chronic kidney disease all carry inflammation with them. But according to a 2019 study more than 50% of all deaths stem from chronic inflammatory conditions.
Here is a more complete list of what type of clinical conditions are associated with chronic inflammation:
- cardiovascular disease, such as heart disease and stroke
- obesity
- cancer
- chronic obstructive pulmonary disease
- asthma and allergies
- diabetes
- chronic kidney disease
- chronic pain — for example, from some sources of back pain, headache disorders, arthritis and other joint conditions
- non-alcoholic fatty liver disease
- autoimmune diseases, such as rheumatoid arthritis, lupus, ulcerative colitis, and Crohn’s disease
- depression
- neurodegenerative conditions, such as Alzheimer’s disease
Some people may have two or more of these chronic diseases at the same time. This increases the risk of death. This is even more of a reason to follow an anti-inflammatory diet.
Anti-inflammatory diet
The CNN article suggests that an anti-inflammatory diet has the potential to reduce inflammatory cytokines. This is important and can also improve symptoms of chronic inflammatory diseases. A large study was conducted in 2021, which showed that people on an anti-inflammatory diet had a lower probability to get complications. Anti-inflammatory diets protected them from heart attacks, strokes, coronary heart disease and more.
Here are the ingredients of an anti-inflammatory diet
Why are anti-inflammatory diets so healthy? It is because they are rich in fiber, omega-3 fatty acids, antioxidants, polyphenols, vitamins, and unsaturated fats can have anti-inflammatory effects. Fruit options can include:
- apples
- fruits with stones or pips, such as peaches, plums, apricots, and cherries
- grapes
- citrus fruits such as oranges, lemons, limes, and grapefruit
- pomegranates
Vegetables are high in fiber and other important vitamins and nutrients. Include a variety of colors of vegetables in your daily diet. Options can include:
- green leafy vegetables, such as spinach, kale, radicchio, and arugula
- cruciferous vegetables, such as broccoli, cauliflower, cabbage, and brussels sprouts
- tomatoes
- root vegetables, such as turnips, beets, radishes, and onions
- potatoes
- sweet potatoes
Whole and cracked grains are another source of fiber.
Nuts and seeds
Nuts and seeds contain polyphenols, which can have an anti-inflammatory effect. Nuts and seeds can include almonds, peanuts, cashews, hazelnuts, flaxseeds, sesame seeds, chia seeds, sunflower seeds, and pumpkin seeds.
Healthy oils
Vegetable oil like olive oil are important for cooking and for salad dressings.
Fish
Fish that is high in fatty acids and omega-3s can be important in an anti-inflammatory diet. These fish varieties can include salmon, tuna, sardines, and mackerel.
Herbs and spices
Some herbs and spices may have anti-inflammatory effects, as they can be high in phenols and antioxidants. These include clove, sage, oregano, cinnamon, rosemary, turmeric, black pepper, and ginger, among other options.
What to avoid
Highly processed foods like hamburgers, french fries, cakes and others must be removed from your food list. They are associated with heart attacks, strokes and cancer. In addition, the following food component must be avoided, if you value your life.
- Refined carbohydrates: This can include products made with white flour, such as white bread, pasta, breakfast cereals, and pastries.
- Trans fats: These can include foods labeled as having partially hydrogenated oils in them. Examples include baked goods such as cakes, pies, and frozen pizzas, as well as fried foods such as donuts or fries.
- Some saturated fats: red meat, chicken with the skin on, milk, cheese, and cream contain high levels of certain saturated fats that promote inflammation.
- Sugar: Sugary foods or foods with a high glycemic index can be inflammatory. Examples can include sugary drinks and sodas, sugary cereals, and candy.
- Red meat and processed meat: This can include beef, lamb, goat, and pork meat, as well as processed hot dogs and sausages, among others. These meats have an association with colorectal cancer.
- Certain spreads and cooking fats: Some fats such as margarine, shortening, and lard can be inflammatory.
Conclusion
You hear bad things about chronic inflammation and premature deaths. What you may not have heard a lot yet is that anti-inflammatory diets actually can safe lives. Above I have listed the most common inflammatory diseases. I also described the ingredients of an anti-inflammatory diet. With this diet researchers found that cardiovascular disease was reduced by 38%, strokes were reduced by 28%. It is not that difficult to adopt a healthy anti-inflammatory diet. Keep trans fats and highly processed foods away. Eat more vegetables, fish and avoid red meats. Add some nuts and cold pressed extra virgin olive oil. Good health will thank you for this diet change.