Many people sleep throughout the night, but do you wake up every night at 3 AM? This article will explain to you what to do. A recent article of CNN Health reviewed why this happens in some people and what you can do about it.
Nocturnal awakenings are common. Waking up several times during the night occurs naturally between sleep cycles. However, these awakenings last only a few seconds to a few minutes, and then we fall asleep again. A complete sleep cycle takes between 90 and 110 minutes and consists of 4 stages.
It is during the fourth stage, the rapid eye movement (REM) stage that your sleep is lighter and you can wake up briefly. This is normal, if you fall asleep again after. As long as you are not hungover the following day, there is no concern regarding this.
Problematical nightly insomnia
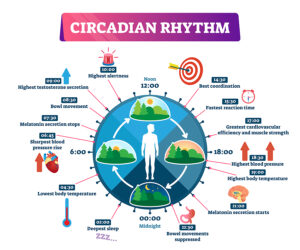
However, a small percentage of people wake up around 3 AM every night and have major problems falling asleep again. They may stay awake for 1 or 2 hours and they get a “hangover” the following day due to the missing sleep. Often they may require a nap in the following afternoon to catch up with the sleep deprivation. Dr. Cathy Goldstein, a professor of neurology at the University of Michigan in Ann Arbor said: “Circadian rhythm is our internal biological clock, it times when we’re awake, it times when we’re asleep — it times most of our physiological processes, so our body does what it needs to do at the right time of day.”
Night owls and early birds
She went on to say: “Circadian rhythms and sleep architecture change with age, which might be why someone would feel like they received more deep sleep when they were younger. As people age, they tend to spend more time in light stages of sleep.” There are also other sleep behaviors such as night owls and early birds. It is the night owls who go to bed late, which change their circadian rhythms. This can result in light sleep, more nighttime awakenings and daytime sleepiness.
What to do when you have problems falling back to sleep
The key to rectify a changed circadian rhythm is as follows.
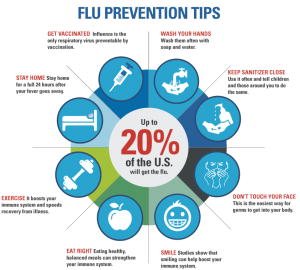
- Always go to bed between 10 PM and 11 PM, which will set the circadian rhythm.
- Have natural light exposure during the day and have no artificial lights in the bedroom during the night.
- Make sure the room temperature is cool and there is no noise exposure in the bedroom.
- Use a low dose melatonin supplement in the night, if you cannot return to sleep right away in the middle of the night.
- If you cannot go back to sleep within 15 minutes, get up to avoid associating your bed with wakefulness. Listen to relaxing music or meditate.
- Goldstein said: “If the awakening is naturally caused by your sleep architecture and does not affect how you function the next day, there is nothing to worry about.”
Conclusion
Do you wake up every night at 3 AM? A small percentage of people do. As long as we fall asleep right away this is normal. But, if we stay awake for 1 or 2 hours, we need to do something about it. In order to establish a healthy circadian sleep rhythm, we need to go to bed around the same time of the evening, preferably between 10 and 11 PM. We need to have natural light exposure during the day and have no artificial lights in the bedroom. Make sure the room temperature in the bedroom is cool and there is no noise exposure. Use a low dose melatonin supplement in the night, if you cannot return to sleep. If you cannot go back to sleep within 15 minutes, get up to avoid associating your bed with wakefulness. Listen to relaxing music or do meditation.
Establishing a “sleep hygiene” with habits like avoiding stimulation and replacing it with relaxation before going to sleep is a good first step to a more restful night.