In this month’s Lancet Oncology Manit Arya et al. have reviewed the research and clinical achievements of Harvard Medical School trained Charles Huggins. This Canadian-born American surgeon won the Nobel Prize in Physiology and Medicine in 1966 for his outstanding research on treatment of prostate cancer. Here are the key findings of a publication in 1941 by Huggins and Hodges: 1. Prostate cancer is a cancer that is hormone controlled 2. Prostate cancer that has spread to other organs can be inhibited in growth by removal of testosterone production (surgical removal of testicles or orchiectomy) or by treating with female hormones (estrogens). 3. Prostate cancer that has spread to other organs is made to grow faster, if testosterone is injected. The authors of this review pointed out that despite hundreds of further research papers these “original studies have withstood the test of time”.
Estrogen treatment has caused cardiovascular and thromboembolic complications, which resulted in cessation of this treatment modality. Newer studies attempted to improve prostate cancer survival with synthetic luteinising-hormone-releasing-hormone (LHRH) agonists and various antiandrogens, but nothing compares to the survival success of a simple orchiectomy. The authors concluded that Huggins and Hodges have provided an “epic work”, which will stand out from the myriad of publications in science for “years to come”.
Manit Arya, Dr, FRCS, Iqbal S Shergill, FRCS, Philippe Grange, MD, Mark Emberton, FRCS , The Lancet Oncology – Volume 9, Issue 11 (November 2008)
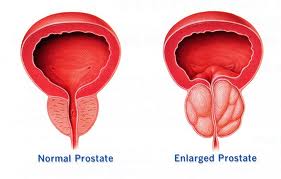
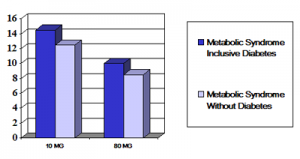
Comment on Nov. 18, 2012: Unfortunately this type of research has confused the treatment of prostate cancer for decades. I have explained this in detail under this link: http://www.nethealthbook.com/articles/cancer_prostatecancer.php#introduction It turns out that the precise opposite is true: The aging male who is most prone to develop prostate cancer needs testosterone replacement, as prostate enlargement and prostate cancer is due to a LACK of testosterone, which causes estrogen dominance. This hormone scenario takes place in the aging male, if not corrected! This type of patient would need an understanding urologist as explained under the link above. Unfortunately many physicians, including famous ones are slow to adapt to new knowledge from their peers (in this case Harvard trained Dr. Abraham Morgentaler, an urologist who is cited under the above mentioned link).
Last updated December 3, 2012