Pre-eclampsia is a condition, which can threaten a woman’s health and also the unborn baby. It can occur in the second and third trimester. These latter stages of pregnancy (there are 3 stages) are where the doctor should check for early pre-eclampsia signs. In the past this would go unchecked and develop to the full-blown condition of eclampsia and be a significant cause of maternal mortality rate
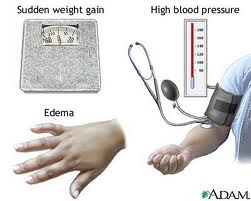
and fetal mortality rate. With prenatal visits and check-ups the early signs are easily recognized: the pregnant woman would complain that her rings would not fit her any more. Significant weight increase due to fluid retention where her legs and the area of her shinbone would be puffy, is called edema. The dipstick test would tell more: it would indicate the presence of protein in the urine sample. These changes are a cause of high blood pressure, which is another important clinical sign and can be readily checked. For these reasons it is imperative that regular pre-natal visits take place at the doctor’s office.
Pre-eclampsia occurs, when substances are released from the placenta into the bloodstream of the mother, and they affect the kidneys. If the condition progresses to eclampsia, it can lead to kidney damage and seizures, and the outcome will be fatal.
For a long time it was a puzzle to physicians, why some women would show pre-eclamptic symptoms and others would remain problem-free.
New research on patients’ medical history from the John Radcliffe Hospital, Department of Obstetrics and Gynecology in Oxford, Great Britain has been able to point out predisposing risks for pre-eclampsia in pregnant women.
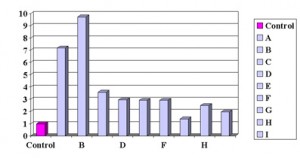
A family history and history of previous eclampsia increases the risk, but also certain health problems make it more likely that pre-eclampsia will occur in the later stages of pregnancy: diabetes mellitus, kidney disease and high blood pressure are medical conditions that increase the risk. Beside these health conditions an increased body mass index at the start of pregnancy can be a predisposing factor, and a high maternal age-women over 40 years of age- are more likely to have the complication of pre-eclampsia. It is obvious that the risk gets higher, if several of these predisposing factors are present. The highest risk is found in women with a rare inherited variation of lupus, called anti-phospholipid syndrome, where blood clots are a problem and pre-eclampsia is a high risk with pregnancy.
Risk Factors For Pre-Eclampsia According To Meta Analysis (published
|
| Explanation of independent risk factors: A= Previous History Of Pre-eclampsia; B= In Women With Anti-Phospholipid Antibodies; C= Pre-existing Diabetes; D= Twin Pregnancy; E= First Child; F= Family History; G= High Blood Pressure; H= High Body Mass Index; I= Maternal Age 40 or more |
While it is absolutely imperative that regular pre-natal checks are part of proper health care, there are other consequences. There would be reason to be especially watchful with predisposing conditions. Last not least, prevention also has its place.
It is important that health concerns are already addressed as part of planning for a healthy pregnancy. Avoidance of alcohol and quit smoking are of extreme importance, followed by achieving a normal weight. Good eating habits are needed throughout the entire pregnancy. Opting for pregnancy after age 40 seems trendy in some celebrity circles, but with the knowledge of risk factors, it should be looked at with caution. Nature equipped the human species to have children in the age of 20 to 30, and even though a forty year old may have a youthful appearance, the genetic material is aged, and the biological clock cannot be fooled. Prevention also means that any health condition like preexisting diabetes should be well controlled before a pregnancy.
With a proactive and common-sense approach pre-eclampsia can be either avoided or recognized and treated early, resulting in healthy outcome for mother and baby.
More information about high risk pregnancies: http://nethealthbook.com/womens-health-gynecology-and-obstetrics/pregnancy-labor-delivery-2/%20High%20Risk%20Pregnancies/
References: British Medical Journal 2005;330:565(12 March)
Last edited October 28, 2014