This article is about news from the Blue Zones regarding longevity. Blue Zones are areas where many centenarians live. Medical News Today ran a review article about Blue Zones on Sept. 23, 2023. These Blue Zones are located in Sardinia, Italy; Ikaria, Greece; Nicoya, Costa Rica; Loma Linda, California and Okinawa, Japan. Many studies looked at centenarians in these areas and analyzed what lifestyles led to their longevity. Dan Buettner summarized at a conference that only 20% of deaths in the world are due to genetic conditions. 80% of people can postpone their death date by adopting healthy lifestyles.
Factors associated with longevity
Dan Buettner called the factors that lead to prolonged life “Power 9”. The following factors must be adopted simultaneously, if you want to reach 100 years of age and more:
- Moving naturally and regularly
- People in Blue Zones have a purpose in life
- Reduce stress in your life
- Practice the 80% diet rule, which is to stop eating when 80% full
- Adopt a plant-based diet.
- Consume alcohol in moderation
- Be part of a community
- Put family first
- keep a social circle that supports healthy behaviors
A diet for longevity
Dan Buettner analyzed the dietary habits of centenarians. He found that 90% of the diet they consumed consisted of whole food, plant-based sources and about 65% of their diet were complex carbs. Buettner noted: “The pillars of every longevity diet in the world are whole grains, nuts, greens, and other garden vegetables, tubers and beans.” For years the benefits of a Mediterranean diet were investigated and found to be life prolonging. It also emphasizes vegetables, whole foods, greens, grains, nuts and beans. The review article in Medical News Today that I mentioned above contains recommendations of how to change your diet to a healthier one.
Regular exercise
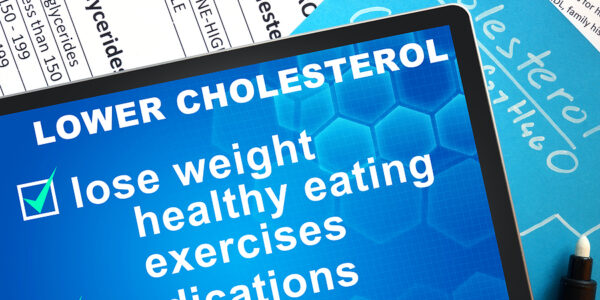
We are built in a way that requires regular exercise. When you exercise regularly, your body produces healthy HDL cholesterol that balances the unhealthy LDL cholesterol. Overall, this counteracts clogging of arteries and prevents heart attacks and strokes.
When you prevent strokes and heart attacks, you live longer.
Have a purpose in life
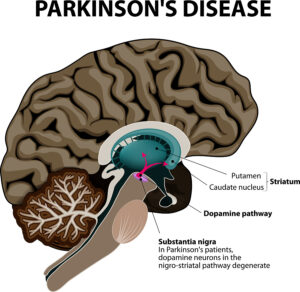
When you have a purpose in life, your mind is focused on what excites you. Achieving what is your dream satisfies you. Your brain releases feel-good brain hormones (dopamine, serotonin, endorphins, and oxytocin). When these hormones are released, you relax and cope with stress better. Your blood pressure normalizes, hardening of the arteries is postponed. At the same time, you prevent heart attacks and strokes. This contributes to longevity.
Reduce stress in your life
When under stress, your adrenal glands release adrenaline and cortisol. In the short term these stress hormones help you to cope better with stress. But when stress gets chronic, it weakens your immune system and increases your risk for a heart attack or stroke. It ages you faster. You can counter stress in your life by adopting stress management techniques. Regular exercise stabilizes your emotional life. You can listen to relaxation recordings or to relaxing music to calm your nerves. Developing friendships is another method of coping with stress. Here is more information on how to reduce stress in your life.
Limit alcohol consumption
In the past it was thought that small amounts of alcohol would prevent cardiovascular disease. But these studies overlooked the fact that even small amounts of alcohol can cause various cancers. So, by limiting the amount of alcohol consumption you also limit your probability of getting cancer.
Be part of a community
Many psychological studies showed that social isolation leads to health problems. It follows from this that being part of a community stabilizes your health and prevents disease. When you socialize with other people you counter stress and prevent loneliness.
Putting family first
When you care about your family, family members will care about you. Studies showed that this is an important factor in preventing disease. It even reduces mortality. Lower mortality leads to longevity.
Keep a social circle that supports healthy behaviors
Strangely enough here is another psychological factor that leads to longevity: getting support from a social circle. Being part of a social circle can create positive energy that prevents health problems.
Discussion of factors that lead to longevity
It is interesting to see that a lot of the longevity factors are psychological in nature. But physical factors are also important, like a Mediterranean diet and regular exercise. One factor that was not mentioned by Dan Buettner is the importance of preservation of hormone stability. I attended many yearly conferences of the American Academy of Anti-Aging Medicine (also known as A4M). They take place in the middle of December in Las Vegas every year. Over the years many lectures centered around hormone deficiencies. They collectively lead to premature aging and deaths. However, speakers also stressed that when you replace the missing hormones, you can reach a balance point where life gets prolonged.
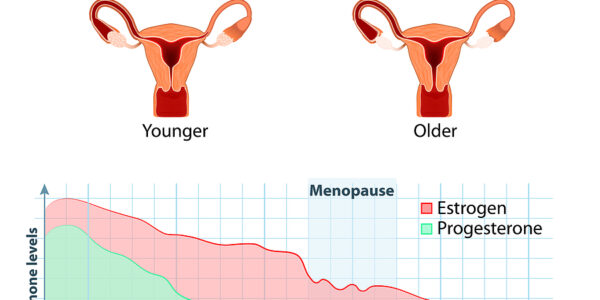
Hormone replacement
One of the speakers, Dr. Hertoghe, an endocrinologist from Brussels mentioned in various talks that a lack of human growth hormone (HGH) in older age can lead to premature death. When IGF-1 levels in the blood are low, replacing the missing HGH with regular HGH injections can add 26.5 years to your life expectancy. But other hormones like thyroid hormones, testosterone in males, and progesterone and estrogen in females can prolong life when replaced after menopause or andropause (the male version of menopause).
Conclusion
Many factors contribute to longevity in centenarians. A lot of the factors are psychological in nature, like having a purpose in life or reducing stress in your life. Others are: be part of a community, put family first and keep a social circle that supports healthy behaviors. Physical factors causing longevity are moving naturally and regularly; adopt a plant-based diet; and consume alcohol in moderation. There is one important factor of longevity that Dan Buettner overlooked: your hormone balance. When we approach age 60 and beyond many people stop producing adequate amounts of hormones.
Replacing missing hormones
Anti-aging doctors have done studies showing that replacing missing hormones in proper doses will prolong life. Dr. Hertoghe, an endocrinologist from Brussels mentioned in various talks that a lack of human growth hormone (HGH) in older age can lead to premature death. When IGF-1 levels in the blood are low, replacing the missing HGH with regular injections can add 26.5 years to your life expectancy.