,You can get dementia and strokes from diet drinks. This is what a recent study published on April 20, 2017 in the American Heart Association Journals has shown. Because of the bad press around sugary drinks more and more people have switched to diet drinks. But the authors of this study have found a correlation of consuming diet soft drinks (with artificial sweeteners), dementia and ischemic strokes.
How was the study done?
The community-based Framingham Heart Study followed patients on diet soft drinks for 10 years. There were two age groups: mean age of 62 and mean age of 69. There were 2888 participants in the younger age group and 1484 participants in the older age group. Researchers observed the younger age group for strokes, the older for dementia. During the observation time there were 97 cases of stroke (82 of them ischemic) and 81 cases of dementia (63 due to Alzheimer’s disease). In comparison to the controls with no consumption of diet drinks, there was an increase of 296% of ischemic stroke and 289% increase of Alzheimer’s disease. This was the data consuming diet soft drinks for 10 years. Another control group had consumed sugar-sweetened beverages. They did not develop strokes or dementia (observation time too short). As can be seen under this link the popular press also reviewed the study.
What do we know about artificial sweeteners?
Here is a brief review of the most common sweeteners.
1. Saccharin
This sweetener’s history goes back to 1879 when the Russian chemist Constantin Fahlberg first noted experimenting with coal tar compounds that one of the end products, benzoic sulfanide, tasted sweet. In fact it was between 200 and 700 times sweeter than granulated sugar! But there were political struggles that accompanied this saccharin throughout the years. There were rumours that in rats saccharin could cause bladder cancer. The health authorities became concerned. This led to Congress passing the Pure Food and Drug Act in June of 1906, to protect the public from “adulterated or misbranded or poisonous or deleterious foods, drugs or medicines.”
The origin of the FDA
This was the precursor of the FDA that would examine all of the medical evidence and consider the pros and cons of sweeteners as well. President Roosevelt took saccharin for weight control to replace sugar. In 1908 Roosevelt felt he had to stop the actions of overzealous Dr. Harvey Wiley, chief of the U.S. Department of Agriculture’s chemical division who was of the opinion that saccharin should disappear from market. Dr. Wiley did not give up his fight and finally the FDA decided to ban saccharin in processed foods, but to continue to allow private sales of saccharin.
2. Cyclamate
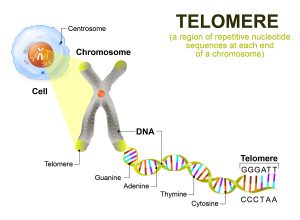
Cyclamate first appeared in 1937. The company marketed the sweetener initially to achieve better control of blood sugars in diabetes. Because of the reduction in sugar consumption it allowed diabetic patients to cut the amount of insulin required to control diabetes. Cyclamate did not have a bitter aftertaste, so in a marketing move the company mixed cyclamate with saccharine. The ratio was 10 parts of cyclamate to 1 part of saccharin , which resulted in the creation of “Sweet ‘N Low. In 1958 the FDA gave cyclamate the GRAS designation: “generally recognized as safe”. The good fortunes of cyclamate did not last long: in 1969 damaging animal experiments showed that cyclamate/saccharin had caused chromosomal breaks in sperm of rats. Another study from 1970 showed bladder tumors in rats. Other studies showed lung, stomach and reproductive tumors in animal experiments with cyclamates/saccharin.
History of Sweet N’ Low sweetener
The FDA wanted to shut down the sale of the Sweet N’ Low sweetener, but public pressure and the food processing industry forced the issue to be brought up in front of Congress. The compromise was to use a warning label: “Use of this product may be hazardous to your health. This product contains saccharin which has been determined to cause cancer in laboratory animals.” In the year 2000 and beyond researchers did several animal experiments. The data from Denmark, Britain, Canada and the United States on humans showed no signs of bladder cancer from exposure to Sweet N’ Low. In 2000 Congress removed the warning labels.
3. Aspartame
The detection of aspartame occurred in 1965. James M. Schlatter, a chemist, was looking for anti-ulcer drugs, but noticed the intensely sweet flavor when he licked his fingers. This led to the newest sweetener by 1973. We know it by the trade names Equal, NutraSweet or Sugar Twin. As this sweetener consists two amino acids, phenylalanine and aspartic acid. The body metabolizes it except people with phenylketonuria, with certain rare liver disorders or pregnant women. High levels of phenylalanine occur in their blood, because they cannot metabolize aspartame properly. Any food made with aspartame has to carry that restriction on the label, a requirement by the FDA.
Problems with Aspartame
In 1996 W. Olney and his associates presented research that implied that Aspartame would have caused brain tumors in rats. But later these experiments were disproven and studies from children with brain tumors showed “little biological or experimental evidence that aspartame is likely to act as a human brain carcinogen.”
4. Sucralose
The history of sucralose goes back to 1976 when insecticide researchers looked for new types of insecticides. They found that chlorinated sugar worked as an insecticide. One of the researchers tasted sucralose and to his surprise it was very sweet. If you Google “Splenda and insecticide”, you have a hard time finding references regarding the history of sucralose, but 20 years ago I found a detailed description that explained how one of the chemists doing insecticide research accidentally tasted one of the research products, and it was about 600-times sweeter than table sugar.
Sucralose kills ants
Here is one of the few references that explains that sucralose was discovered while looking for new insecticides. I have repeated the insecticide experiment myself in Hawaii where small ants are ubiquitous. Out of curiosity I took a package of Splenda from a coffee shop and sprinkled the contents in the path of ants. In the beginning the ants were reluctant to eat it, but after a short time they came and took it in. They slowed down, and finally they were all dead. A few hours later the only thing visible were dead ants that were only 1/3 of their original size. This was proof enough for me that Splenda, which originates from insecticide research, is not suitable for human consumption.
Side effects of sucralose in humans
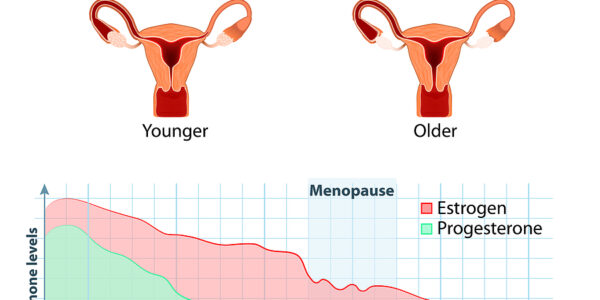
In the meantime Dr. Axe in the above references lists the side effects in humans: “Migraines, agitation, numbness, dizziness, diarrhea, swelling, muscle aches, stomach and intestinal cramps and bladder problems.” In the Splenda marketing scheme they decided to first introduce Splenda gradually into diabetic foods as a sweetener, then later sell it to the public at large. Don’t fall for it! It was a side product of insecticide research, and insecticides have the undesirable quality of being xenoestrogens, which block estrogen receptors in women. As a result estrogen can no longer access the body cells, including the heart. The final consequence for a woman is a higher risk for cardiovascular disease. This can cause heart attacks, strokes and cancer. In men estrogen-blocking xenoestrogens can cause breast growth and erectile dysfunction. Taken everything together Splenda seems to be too risky for its sweetness.
5. Other sweeteners
Other sweeteners researchers have not stopped looking for newer, better sweeteners. There is a number of sugar alcohols with less calories than sugar such as erythritol. Another common sugar alcohol is xylitol, used in chewing gum. The advantage is that these are natural sweet alcohols that exist in nature. Xylitol originated from birch wood and the general opinion was that it was useful to fight tooth decay. Manufacturers of chewing gum mixed xylitol into some of their products. Karl Clauss and Harald Jensen in Frankfurt, Germany detected another sweetener, acesulfame potassium, also known by the names acesulfame K, Ace-K, or ACK in 1967 when they experimented with various chemicals. This is known under the brand name “Sweet One”, but is often disguised in processed foods together with other artificial sweeteners to mimic the taste of sugar.
6. Stevia
Stevia has been used for over 400 years, particularly in South America. It grows like a small bushy herb with leaves that can be taken to sweeten foods. With modern, reliable extracting procedures (Sephadex column) it is possible to separate the bitter component of stevia and discard it leaving stevia behind without any bitter aftertaste. Stevia occupies 40% of the sweetener market in Japan. In Europe and North America there is a lot of competition with the above-mentioned sweeteners, mainly because of clever marketing techniques. The FDA gave stevia GRAS status in 2008.
What does sugar in soft drinks do?
Sugar is an emotional topic that can get people caught up in heated discussions. The sugar industry and the sugar substitute industry have also powerful lobby groups that provide the Internet and the popular press with conflicting stories to convince you to buy their product. There is good data to show that sugary drinks cause heart attacks, strokes and diabetes. Let’s not forget the metabolism behind the various sugars and starchy foods leading to fat deposits, high triglycerides and high LDL cholesterol.
Cut out sweets, cut out artificial sweeteners, but you can use stevia
Forget the emotions of severing yourself from your favorite fix. Instead replace the familiar sweet taste you are used to from childhood on with stevia. At least this is what I do. The only alternative would be to take the plunge and cut out any sweet substance altogether, which I am not prepared to do. If you can do it, by all means go ahead. For more details regarding the effects of sugar and starchy foods read the blog under this link.
Conclusion
Diet soft drinks have become very popular. The reason is that studies in the past showed that sugary drinks can cause heart attacks and strokes. Now a new study revealed that diet soft drink consumption is associated with dementia and strokes. These drinks contained saccharin, cyclamate, aspartame or sucralose. They did not contain stevia, a natural sweetener because it is a natural, not a patented sweetener. It seems that companies’ profits are higher with chemical, patented sweeteners.
The problem with manufacturers and the FDA regulatory body
Looking back in time it seems perfectly legal that a company produces a chemical, patents it and sneaks it through the FDA channels for approval. The company then markets diet soft drinks turn out later to produce dementia and ischemic strokes in much larger studies. The FDA originally based their judgement on much smaller experiments for the initial approval. I have noticed that companies are now quietly introducing stevia, a natural sweetener to avoid potential legal problems down the road. Perhaps it is time to follow the Japanese lead where stevia is already occupying 40% of the sweetener market.