Although people increased the use of brain stimulating substances in the last 17 years, nobody paid attention to the situation, when natural substances turn into poison. The Center for Injury Research and Policy and the Ohio State University College of Medicine, both in Columbus, OH conducted a study. The researchers looked at the use of natural substances from 2000 to 2017. They noted that during this time marijuana had increased by 150% and there was a 64% increase of nutmeg use. Nutmeg contains the hallucinogenic substance myristicin, a potent mind-altering substance. There was a 4949% increase of kratom use, which comes from the leaves of a South American tree which have powerful mind-altering substances. The original study of the researchers was published here.
More hallucinogenic substances
Other natural substances came from Jimson weed, where the leaves and seeds contain natural substances that cause hallucinations and euphoria. It contains the chemicals atropine, hyoscyamine, and scopolamine. These interfere with the normal messenger molecule acetylcholine in the brain and in nerves. 21% of all toxic reactions between 2000 and 2107 were due to Jimson weed. Besides those, 16% of all toxic reactions came from magic mushrooms. There are other natural substances which are similar. They come from a shrub that grows in East Africa and southern Arabia. Khat contains the alkaloid cathinone, which is a stimulant. It causes excitement, loss of appetite, and euphoria.
More details about the different natural substances and their actions
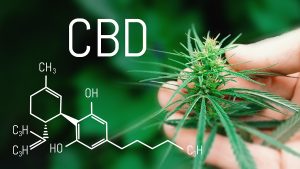
Marijuana
Marijuana includes dried leaves, the stem, seeds and flowers of the Cannabis sativa or Cannabis indica plant. The mind-altering THC compounds are what people are seeking out. When a person smokes marijuana, the THC enters the blood through the lungs. The THC reaches the brain and causes a “high”. This can be associated with seeing brighter colors, get an altered sense of time, have hallucinations, delusions and in severe cases a psychosis. Marijuana peaks at different times depending on whether it is smoked or taken in as an edible. When smoked, the effect of marijuana is felt by the user within a few minutes. Ingested as edibles will take 30 minutes to one hour to show an effect, but it lasts a lot longer (3 to 4 hours). This is important to know, particularly if other agents including alcohol are combined with marijuana.
Nutmeg
Nutmeg is used in small amounts as a spice, typically ¼ to ½ teaspoon in a family dinner. However, when a person consumes 2 teaspoons or more of nutmeg, such as more than 10 mg, toxic symptoms occur. Symptoms from myristicin, the active substance in nutmeg, can be hallucinations, dizziness, confusion and seizures.
Kratom
Kratom is a tropical tree (Mitragyna speciosa), which is native in Southeast Asia. The leaves contain mind-altering compounds. At this time kratom is freely available on the Internet. There is no restriction in the US. But there are health concerns. Kratom has both opioid and stimulant effects on the brain. It produces sensations of pleasure, sedation and decreased pain. In small amounts people experience increased energy, sociability and alertness. There are a number of side effects: nausea, sweating, itchiness, dry mouth, increased urination, constipation, loss of appetite, hallucination and seizures. Kratom caused 8 of the 42 deaths reported by the Ohio State University College of Medicine, Columbus, OH study.
Jimson weed
The leaves and the seeds of Jimson weed are used by drug-seeking individuals. It causes hallucinations and euphoria, a heightened sense of well-being. It contains the chemicals atropine, hyoscyamine, and scopolamine. These interfere with acetylcholine, one of the major hormones in the brain and nerves. 15-100 grams of leaf and 15-25 grams of the seeds can be lethal. Children are more sensitive, so the lethal dose is much smaller for them. Jimson weed slows down the stomach emptying and also the activities of the large intestine leading to severe constipation. It can cause glaucoma and also rapid heartbeat. Urinary retention is also common.
Khat
Khat is a drug found in the wild East African shrub called Catha edulis. It contains a central nervous system stimulant, called cathinone. People living on the Arabian Peninsula are chewing the leaves of this plant. It is illegal in Canada and the US. In Ethiopia 30% of adolescent girls and 70% of the adolescent boys chew khat. The effect of khat is similar to the effect of a strong coffee. It has a stimulant effect like the coca plant that is used to make cocaine. It increases respirations, elevates blood pressure and leads to gum disease. This results in tooth decay. Ulcers and constipation occur more often. People on khat become more talkative, elated and euphoric. Some say that they have more imagination and are able to associate things better. From a medical point of view Khat causes constipation, hemorrhoids and impotence. Other symptoms are blurred vision, headaches and dizziness.
Kava kava
Piper methysticum, a plant native to the western Pacific Islands is from which kava kava is made. Kava kava relaxes you, but it has caused liver damage and is even responsible for a few deaths. It has been banned from many European countries and Canada. It is still available in the US. Some people take kava kava for sleeping problems, anxiety and restlessness. There are many more claims that kava kava is effective for other diseases, but research could not confirm those claims. Kava kava is detoxified in the liver, but in doing so there are profound interactions with other drugs that get detoxified in the liver. This liver toxicity has led to irreversible liver damage requiring a liver transplant. Several people have died because of liver failure.
Magic mushroom
Wild mushrooms, namely magic mushrooms that contain psilocybin are a popular way to get a high. Psilocybin is psychoactive and hallucinogenic. Psilocybin is classified as a Schedule I drug in the US, meaning that it is highly addictive, but has no currently accepted medical use for treating any medical condition. Magic mushrooms cause nausea, yawning, drowsiness, nervousness, panic, paranoia, hallucinations and psychosis.
Toxic side effects of natural substances reported to Poison Control
There were 67,369 calls to poison control centers in the United States between January 1, 2000 and December 31, 2017 regarding natural substances. This is when natural substances turn into poison. There were 41.4% from calls regarding older than 19-year-old individuals. 34.8% of calls to the poison control center was regarding the age group between 13- and 19-year olds. 46.9% of cases were due to marijuana, 21.1% of the calls to the poison control centers were due to anticholinergic plants, 15.6% were due to hallucinogenic mushrooms. In the age group of 3-19 years 47.8% called because of marihuana overdoses. Above the age of 19 it was 53.0% who overdosed on marijuana. In children less than 6 years of age 44.4% of toxic overdoses came from anticholinergic plants.
Deaths reported in the study
The study reported 42 deaths from 2000 to 2017. 8 deaths were due to kratom. 7 deaths among the 42 deaths occurred in people under the age of 18. 5 of the 42 deaths occurred in teenagers aged 13 to 19. Two of the deaths occurred in children under the age of 12. These were due to marijuana.
Discussion
When reviewing the research of natural substances with the potential to cause addiction, it is important to see things in the right perspective.
Natural substances can be poisonous for you
Many people think that a natural substance, like a leaf from nature, should be trustworthy. But it is the chemicals that people swallow, inhale or chew that matter. Opium also comes from a “harmless” poppy seed. But opium is a powerful and addictive substance. All of the natural substances reviewed above contain potent mind-altering agents. This means that the natural substances are not safe.
Using SPECT scan to measure brain activity
None of the above-mentioned natural substances are harmless. They all attack the brain and interfere with the action of the natural brain hormones in the brain. This may be reversible for a few weeks, but eventually it leads to a chemical burn with permanent damage to the brain. This is when natural substances turn into poison. Dr. Daniel Amen, a psychiatrist has developed a scan that will depict changes in the brain in addicted persons. It is called the Single Photon Emission Computed Tomography or SPECT scan. This nuclear medicine scan measures blood circulation of the brain and brain activity. With prolonged use all of the natural substances show a decreased brain activity pattern on the SPECT scan.
Missing toxicity studies about natural substances
Armed with the SPECT scan as a tool and the knowledge that all of the reviewed “natural” substances have toxic effects on the brain makes one wonder how US citizens could willingly consume these substances for the past 17 years. It was probably a mix of curiosity, peer pressure and the fact that these natural substances were readily available, which made many people try them. There is very little research about toxicity in this field. This is only starting now. To my way of thinking this is another warning sign that people should stop their love-affair with mind-altering natural substances.
Conclusion
I have reviewed the thorny issue of natural substances and how they can turn into poisons. All of the substances reviewed affect brain function. This is why people experience hallucinations, elations and euphoria. But this is not real. It is due to the toxic effect of chemicals on the brain.Advertisements promote kava kava as a relaxing substance. But it can damage the liver and as a result several people have died. It is unknown to a large extent how these natural substances interact with other illicit drugs or with alcohol.
It is best to avoid consuming any of these natural substances. Anybody who consumes them is knowingly consuming a poison, and it means that the user will get into health problems…naturally!