Introduction
Recently a low cost cervical cancer screening method was developed in India. About 25% of all invasive cancers of the cervix in the world are contributed from India as screening for cervical cancer is not practiced there on a large scale. Many screening methods for cervical cancer became more elaborate over the years as I describe here.
However, these screening methods are expensive. They require a doctor who does the Pap test (or takes a swab for DNA testing) and a cytological laboratory. In addition, this service requires a gynecology service back up for positive cancer cases. In the Western world these services are in place and are responsible for improved cervical cancer survival rates.
The American Cancer Society (ACS) guidelines
The ACS guidelines state that cervical cancer screening should begin 3 years after the initiation of sexual intercourse. Women benefit from screening every year for the first 3 years. If 3 consecutive screening results were normal, then a Pap test once every 2 or 3 years would suffice. Because of the Pap test the incidence of cervical cancer has continually dropped in the Western world as seen in this image. Compare this to the next link, which shows India as the main part of the undeveloped countries as a graph on top of the graph for cervical cancer incidence of developed countries.
Cervical cancer is due to a chronic HPV infection
With the new insight that cervical cancer is due to a chronic HPV infection, mostly due to strains 16 and 18 there are shifts in screening methods even in the Western world as DNA tests for HPV can identify a high percentage of cases that would otherwise go on to develop cancer of the cervix. However, due to cost issues with regard to DNA testing for HPV the Pap test is still the method of choice in many Western countries including the US.
HPV16 and HPV18 were very prevalent in the cervical cancers found, not only in premalignant lesions, but also in advanced cervical cancer as this study showed. The authors concluded that vaccination with the HPV vaccine (e.g. Gardasil) would have a significant impact on the prevention of cervical cancer, particularly in a country like India where a regular screening program is not yet in place.
An inexpensive test for cervical cancer screening
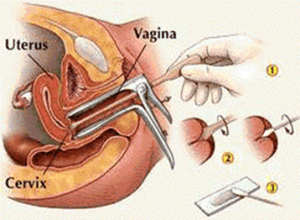
In 2009 there was a publication in the New England Journal of Medicine that investigated three screening methods for cervical cancer, the familiar Pap test (cytology testing), human papilloma virus (HPV) testing and visual inspection after staining with 3-5% acetic acid. In Western medicine the Pap test is done first and if suspicious cancer cells are detected, this is followed up with colposcopy where acetic acid staining is done and a biopsy is taken from the suspicious area. After this one-time test in 1999 the patients of this study received follow-up again (10 year follow-up).
The direct DNA test for HPV
The direct DNA test for HPV caused a 52% reduction of deaths from cervical cancer in comparison to the control group. The other two test methods, done as a single test (cytology testing and acetic acid visualization) did not result in reduced mortality when compared to the untreated control group after 10 years. However, a 15-year follow-up of a one-time screening with the acetic acid test showed a reduction of 31% in the cervical cancer death rate (reduction from 16.2 women per 100,000 to 11.1 women per 100,000) as reported recently at the annual meeting of the American Society for Clinical Oncology. Shastri and co-workers, the authors of this study, estimate that this would translate into prevention of 22,000 cervical cancer deaths annually in India and if instituted across the developing world it would save 73,000 lives annually.
Is cervical cancer screening effective?
A meta-analysis of several randomized studies regarding the effectiveness of cervical cancer screening in reducing mortality from invasive cervical cancer was published in May 2013 and found that cancer screening is indeed very effective.
In most studies Pap tests (cytology testing) or DNA tests for HPV led to a 62% to 65% reduction of mortality from invasive cervical cancer 10 to 15 years later. The protective effect from screening lasted about 5 years. However, the practice of doing Pap tests or DNA/HPV testing every 1, 2 or 3 years is safer than waiting 5 years between tests as there is a cumulative protection to the point of preventing almost 100% of cervical cancer over the years with regular testing.
Staining with 3-5% acetic acid and visual inspection
For India and other development countries the inexpensive visual inspection method to screen for cervical cancer after staining with 3-5% acetic acid is better than not doing any screening at all. A nurse can readily learn this type of screening. Only patients with positive or questionable screening results receive a referral to a treatment center. The best results were possible through a combination of this screening method and vaccinating girls with an HPV vaccine. This leads to a more complete prevention program for cervical cancer in these countries that could otherwise not afford screening. The Bill & Melinda Gates Foundation is helping to reduce the cost of the HPV vaccine to about $4.50 from about $170 in the US, which will allow mass vaccination in development countries in the near future.
What other cervical cancer prevention is available?
As pointed out earlier it is now evident that most cases of cancer of the cervix are due to chronic HPV16 and HPV18 infections. Teens can acquire these and the HPV viruses linger on unnoticed within the affected cervical cells. However, 10 to 15 years later they can manifest themselves as cancer of the cervix . This long latency period allows the physician to screen for this before it becomes invasive and is more difficult to treat. What has become more evident only in the past few years is that other human tissues can get infected with papilloma virus as well and turn cancerous over the years.
Cancers that can occur from sexual contact
Oropharyngeal cancer, anal cancer, penile cancer, vulvar and vaginal cancer and even some forms of throat cancer and lung cancer can develop from intimate contact with a person who is HPV positive. Researchers confirmed that oral cancer is now more than 70% related to HPV infection rather than to cigarette smoking or alcohol as in the past. Sexual practices have changed over the past decades with oral sex being more common. This likely is the reason why HPV caused more oral cancers in recent years.
Finger pointing is not constructive
Finger pointing is not uncommon when it comes to a rational discussion of HPV transmission, but it has become apparent that males are often the ones who may be spreading HPV unknowingly through promiscuous sexual activities. Both heterosexual and homosexual activities will spread HPV. But the more promiscuous a woman is, the more she will also contribute to HPV infections in the population.
HPV vaccines Gardasil and Cervarix
When the pharmaceutical industry developed the HPV vaccines Gardasil and Cervarix many religious groups have spoken out against vaccination, as this would “encourage promiscuous behavior”. I look at this question from the point of view that lives can be saved down the road by preventing several cancers as indicated, and that is what counts on the long-term. In this context it makes a lot of sense that not only females get a vaccination, but also males to interrupt the infectious chain and this trend can now be seen as it is adopted by several jurisdictions.
Conclusion
Cervical cancer screening is still very necessary doing a Pap test or a DNA/HPV test. Screening is necessary more often than every 5 years as pointed out. Most women need a Pap test every 2 to 3 years. HPV vaccination with Gardasil and Cervarix for boys and girls prior to sexual relations is very preventative, but still does not mean that screening should be stopped. Cervical cancer is the cancer that has the longest medical history of moving from a very prominent deadly disease (back in the 1960’s) to a cancer that can now be cured and prevented.
References
- Causes of cervical cancer: http://nethealthbook.com/cancer-overview/cervical-cancer/causes-cervical-cancer/
- HPV vaccine: http://www.mayoclinic.com/health/cervical-cancer-vaccine/WO00120
- Review of cervical cancer: http://www.nethealthbook.com/articles/cancer_cervicalcancer.php#topoftable
Last edited Nov. 7, 2014