In the first place, a large study from Cleveland Medical Center found a connection between Parkinson’s disease and the removal of the appendix. It is important to realize that Dr. Mohammed Z. Sheriff who was the main investigator assembled 62.2 million patients’ records. Of these 488,190 (0.78%) patients had an appendectomy done. 4,470 (0.92%) among these patients went on with a diagnosis of Parkinson’s disease. Of the remaining 61.7 million patients physicians eventually diagnosed 177,230 individuals (0.29%) with Parkinson’s disease. This means that the patients with a prior appendectomy had a 3.17-fold higher risk to develop Parkinson’s disease. Whoever did not have their appendix removed had a lower risk to develop Parkinson’s disease.
Older, smaller studies in the past were ambiguous
A 2016 Movements Disorders study with 1.5 million people in Denmark found that patients who had an appendectomy were a slightly higher risk of developing Parkinson’s disease later in life.
In contrast, a 2018 Science Translational Medicine study found the opposite among 1.6 million Swedes. Patients who had an appendectomy had a lower risk of developing Parkinson’s disease and there was a delay in the onset of it.
It was this discrepancy what motivated Dr. Mohammed Z. Sheriff to design the much larger study that he carried out. He presented the findings at the 2019 Digestive Disease Week meeting that took place May 18–21 in San Diego, CA.
Alpha-synuclein associated with Parkinson’s disease
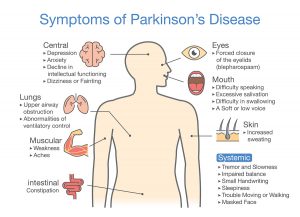
At the same time other investigators found that alpha-synuclein, an abnormal protein in nerve cells, is important for the development of Parkinson’s disease. It plays a role in patients with appendicitis who need surgery. But it also is present in the substantia nigra in the brain of patients with Parkinson’s disease. Notably, patients with Parkinson’s disease often have problems with their balance, muscle rigidly, tremor and slowness of movements.
Indeed, alpha-synuclein has become an important marker for the development of Parkinson’s disease. This publication indicates that monocytes that are activated by the presence of alpha-synuclein can cause significantly more inflammation in the nerve cells of the substantia nigra in the brain. Other authors postulate that oxidative stress in vagal neurons may lead to alpha-synuclein, which can be transported from foci such as in the appendix to the substantia nigra in the brain. More recent studies have shown alpha-synuclein in the gut of patients with Parkinson’ disease according to Dr. Sheriff. In particular, it clearly shows that our gut biome plays a role in the development of disease.
Older people affected by Parkinson’s disease
Certainly, it is mostly people above the age of 60 that come down with Parkinson’s disease. Another key point is that there is no known effective treatment for Parkinson’s disease. However, the new information that alpha-synuclein is a factor in the early stages of Parkinson’s disease is most compelling evidence. By and large, this process leads to toxic clumps of Lewy bodies in nerve cells of the brain and in the gut wall including the appendix. Nobody knows exactly the meaning of Lewy bodies and alpha-synuclein. But if they are playing a part in the initiation of Parkinson’s disease, medications that fight oxidative stress in the nervous system may be a new approach to treating Parkinson’s disease. There is a need for more research.
New approaches to treat Parkinson’s disease
Here is a publication that points out that existing treatment for Parkinson’s disease does not include targeting alpha-synuclein. In the future, these authors state, this will change, as immunotherapy directed at alpha-synuclein will interrupt the development of Parkinson’s disease. Here is another publication that stresses the importance of alpha-synuclein in the development of Parkinson’s disease. It points to testing new therapies in animal experiments and in clinical trials.
Conclusion
The observation that people who had an appendectomy have a 3.17-fold higher risk to develop Parkinson’s disease led to more investigations. It became obvious that an alpha-synuclein accumulation in the nerve cells of the gut wall was playing a role in the disease and formed Lewy bodies. It confirms the concept that disease processes can start with our gut biome. These cells can travel via the vagal nerve into the part of the central nervous system, called substantia nigra. It is there that the dopamine producing nerve cells reside. Destruction of these dopaminergic nerve cells leads to the symptoms of Parkinson’s disease. One of the new approaches to treat Parkinson’s disease is by immunotherapy where antibodies destroy the alpha-synuclein protein. However, clinical trials will have to follow that are testing this new treatment possibility.