When was the last time you saw your physicians for anxiety and you were given a prescription that said: “for anxiety listen to your favorite music!” instead of receiving a prescription for an anti-anxiety drug (anxiolytic). This is exactly what a recent study suggests that showed prior to surgery you can control your anxiety either with anti-anxiety drugs or by listening to your favorite music. Listening to your favorite music will do you no harm, while many drugs do have harmful side effects.
How singing can change the brain chemistry
Other studies have investigated how singing can change your brain functioning in terms of brain chemistry. The researchers found that singing will release dopamine in your brain, which is responsible for feeling pleasure; it will stimulate your immune system by elevating immunoglobulin A and decreasing cortisol (the stress hormone). This in turn will preserve your immune cells (lymphocytes). Oxytocin levels of your brain are increased, which promotes social affiliation. It also calms down the autonomic nervous system resulting in a better airway opening, calming of your heart rate and soothing the wave-like muscle contractions in your gut, medically called peristalsis. You would refer to that as “butterflies in your stomach”. Music therapy reduces pain and anxiety by 50% and is important for children and adults alike.
Pain and anxiety reduced
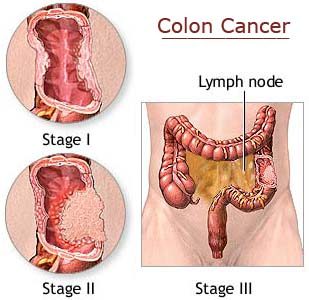
A study in Germany showed that pain and anxiety were significantly reduced with music therapy. A Taiwanese study of women in labor found that music therapy significantly reduced pain and anxiety of women during labor. Ref. 1 explains that music therapy is useful as an adjunct to treating cancer pain, and reducing anxiety associated with colposcopy procedures. It also can help when treating patients who had heart attacks in the setting of a cardiac care unit.
Hypnosis and guided imagery
Music has been successfully combined with clinical hypnosis and guided imagery where words are carefully chosen to help the patient experience pleasant feelings, which counteract the experience of pain, anxiety or fear of dying. A simple relaxation CD or tape with soothing background music will facilitate this type of therapy. This is useful for patients in a palliative care unit where they prepare themselves to accepting the inevitable death from an incurable disease. But chemotherapy patients undergoing these procedures for cancer treatments also have benefitted from a significant reduction in nausea, vomiting (side effects of chemotherapy) and pain.
Autism and music therapy
A Cochrane study showed that autistic children did better in terms of communication skills when music therapy was incorporated into the treatment protocol. One of the core deficits in autistic children is in the area of communication and social skills. This is where music therapy was most effective. Behavioral problems (stereotypic behavior) in autistic children did not respond to music therapy. A comprehensive treatment program for autistic children should therefore incorporate music therapy. Here is a blog that describes what difference music therapy can make in the lives of autistic children written by a member of the American Music Therapy Association.
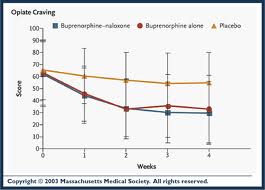
Substance abuse and music therapy
An area where you may not expect music therapy to have a role is in the area of drug and substance abuse rehabilitation , which is discussed in more detail in this site. The beauty about music therapy is that it is not a drug, yet the natural endorphins that are released by the brain help the affected person getting through withdrawal easier. Music therapy helps building up self-esteem, participating in group activities, promoting self awareness and expressing feelings.
Mood disorders in adolescents
One important area where music therapy has been employed is with anxiety and depression in adolescents. Adolescents spend an average of 4 hours per day listening to music. So they are already programmed to listen to music. With the help of a music therapist they can be directed to listening to the type of music that will help them get motivated, relax more, make them feel accepted and be part of their peer groups. In this study the authors suggested to combine music therapy with dance and art therapy. In this way the whole person gets involved in the treatment and this can be integrated with conventional antidepressant treatments at reduced doses (with less side-effects) or with cognitive therapy.
General objectives of music therapy
Music therapy is best incorporated into a treatment protocol as an adjunct. It can help reduce the use of drugs for psychiatric patients, for people with anxiety and for patients with pain conditions. The Cleveland clinic has a useful summary about music therapy, which describes the uses of it for reducing anxiety, for helping with coping skills, mood improvement and distraction from pain. There are registered music therapists you can ask for help. The website of the American Music Therapy Association may have other useful links for you.
Conclusion
Music therapy is a treatment modality with no side effects, but providing effective treatment for quite an impressive range of clinical conditions as discussed. Music therapists are widely available in the US and many other countries. This treatment can be integrated with conventional or complementary treatments. It helps people to heal the body as a whole unit (mind and body).
More information on anxiety disorders: http://nethealthbook.com/mental-illness-mental-disorders/anxiety-disorders-panic-disorders-phobias-ocd-ptsd-anxiety-others/
References
1. Rakel: Integrative Medicine, 3rd ed.© 2012 Saunders. Chapter on Integrative Therapy; subchapter of Mind-Body Therapy.
Last edited Nov. 7, 2014