An important study about the risk of strokes and mini-strokes (called”transient ischemic attacks”) was published in the Oct. 27 edition of the Archives of Internal Medicine. Dr. Daniel J. Bertges and his group followed 1,004 patients between 1988 and 1997 with ultrasound studies of the carotid arteries (carotid artery duplex ultrasound scans). The studies took place at the Pittsburgh Veterans Affairs Medical Center/University of Pittsburgh School of Medicine. Patients were followed with regard to events such as strokes on the side of where the narrowed carotid artery was.
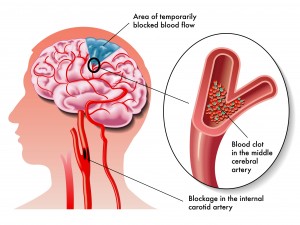
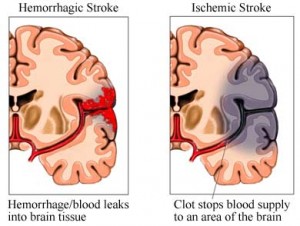
Reversible mini-strokes (medically correct term:”transient ischemic attack” or TIA) were also registered. A total of 1,701 narrowed arteries (called “stenotic arteries”) were found with this ultrasound method. All of the patients initially had no symptoms of the carotid artery stenosis (no dizziness, no fainting, no absence spells or symptoms of TIA or stroke). In 75% of the patients the carotid stenotic lesions were less than 50% meaning that the carotid artery blood flow was acceptable.
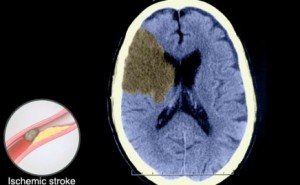
Here are some of the risks as the study went on over the years: both TIA and CVA risk in a given patient occurred at a rate of 3.3% per year. Regarding a specific involved artery the risk of developing a TIA as a result of this was 2% per year and the risk to develop a stroke was 2.1% per year. The investigators found that two main factors determined the ultimate progression into a TIA or a stroke and they were as follows. First, if the artery was severely stenosed at the outset, the probability was high that this would progress and be the cause of a stroke. Secondly, the degree of progression when checked with a follow-up duplex ultrasound was another important factor in terms of leading to a subsequent TIA or stroke.
The composite risk of developing either a TIA or a stroke with a worsening stenotic carotid artery lesion was 1.68-fold. To develop a stroke alone in this scenario the risk was 1.78-fold. Clinical risk factors were of no help in predicting which cases would go on to develop TIA’s or strokes. However, the finding of further progression of a stenotic carotid artery lesion documented on serial duplex ultrasound studies was highly significant.
The authors concluded that there is value in doing serial carotid artery duplex scan studies in the same patient to screen for progressing stenotic lesions in the carotid arteries. When a stenotic lesion is significant enough or progressing fast, intervention by a cardiovascular surgeon with carotid endarterectomy can be done to prevent a stroke or TIA.
Here is a link to a chapter on strokes from the Net Health Book.
Last edited October 26, 2014