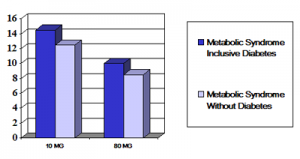
A 5-year multinational prospective study (“Treating to New Targets or TNT Study” involving top cardiologists from around the world has found significant benefits in using higher doses of statins. They investigated the effects of increasing the statin concentration (a cholesterol lowering medication) and have now come to new insights how to approach the metabolic syndrome, which is the metabolic derangement associated with obesity. Of 10,001 patients aged 35–75 years with clinically proven heart disease 5,584 patients had metabolic syndrome at the same time. Half of them were put on 10 milligrams of Atorvastatin (brand name: Lipitor, made by Pfizer Inc.), the other half on 80 milligrams per day. They were followed for 5 years and many questions were asked, blood tests done and statistics kept. Of particular concern was whether survival rates and numbers of heart attacks or strokes would be different for the various groups. The major focus of interest was on people who were over weight or obese.
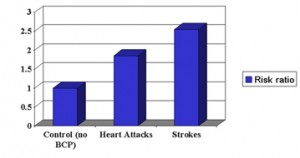
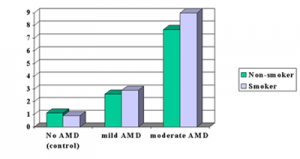
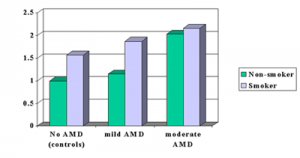
As the image above shows, percentages of complications (heart attacks and strokes) were used as clear end points of cardiovascular complications to measure the response to the statin. The results showed that two subgroups of obese patients, those who have at the same time diabetes and those who don’t, were both benefitting from the higher dose of Lipitor in an equal manner (about a 30% relative reduction of risk).
The amazing result was that dosage of the statin mattered very much. In the past it was thought that taking a pill for high cholesterol was all that mattered. However, now we know that physicians need to watch the blood level response of the bad cholesterol (LDL cholesterol) and titrate the abnormal levels down to a normal level by using adequate dosing. The authors came to the conclusion that metabolic syndrome patients with heart disease, and particularly those where diabetes was present at the same time, would need more intensive statin therapy (higher dosage) than patients who were only having cardiovascular disease. The new goal post for lowering the low-density lipoprotein cholesterol (LDL cholesterol) of 1.8 mmol/L (70 mg/dL) was recommended.
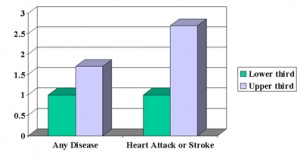
This study showed that there was a 44% increase in absolute risk for an adverse outcome in coronary heart disease patients who also have metabolic syndrome than those without metabolic syndrome. This justifies a very aggressive treatment with Lipitor down to the new target blood values indicated above that your doctor needs to monitor. In high risk patients for heart attacks and strokes where more than 3 cardiovascular risk factors are present the patient’s outlook (longer survival) can be improved by several years. This was shown with treatment using the higher dose of Lipitor when blood levels and cardiovascular complications were compared between 5 years of treatment and the treatment results after the first year of the study.
More information on:
1. Treatment of a heart attack: http://nethealthbook.com/cardiovascular-disease/heart-disease/heart-attack-myocardial-infarction-or-mi/treatment-heart-attack/
2. Metabolic syndrome and obesity: http://nethealthbook.com/hormones/metabolic-syndrome/
Reference: The Lancet 2006; 368:919-928 (09 September 2006)
Last edited November 1, 2014