When your cholesterol is high, what can you do to lower cholesterol? First, there is the bad cholesterol, called LDL cholesterol that should not be too high. Furthermore, there is the good cholesterol, called HDL cholesterol that you want to be to higher to protect you from hardening of the arteries. LDL cholesterol finds its way into plaques of arteries, and later calcification occurs. HDL cholesterol does the opposite; it dissolves LDL cholesterol and brings it to the liver.
Food contributes only to a small portion to the increases of your LDL cholesterol (the bad cholesterol) in the blood. The minor part of the body’s cholesterol stems directly the refined carbs and trans fats from your diet. Here are a number of steps that will protect your heart from LDL cholesterol.
1. Cut out red meat
Cutting out red meat (like beef, pork and sausages) to an absolute minimum, for instance once per week or less is important. The reason is that these meats have more cholesterol in them and also more saturated fats than any other foods. Compare that to poultry, fish and vegetables like beans, which are healthy food sources.
2. Eliminate trans fats
We need to eliminate trans fats as they are causing heart attacks. There is an important difference between ruminant trans fats and artificial trans fats. Ruminant trans fats have been part of the human diet for millennia like milk fat and fat from cows that are on pasture and lamb. Milk products for instance contain fat with 2-5% natural trans fats. 3-9 % of the fat in beef and lamb consists of natural trans fats. Studies have shown that the body is able to handle these natural trans fats and heart attacks are not more frequent in people eating moderate amounts of these products including butter from cows that graze on pasture.
Artificial trans fats
Quite the opposite is true for artificial trans fats in margarine that comes from vegetable oil. Avoid bakery items like sweet pieces or muffins and other products that contain hydrogenated oils. Read labels! Use olive oil or coconut oil, but avoid vegetable oils like corn oil, safflower oil or grape seed oil to get away from trans fats and unstable oils that turn rancid. Rancid oils contain free radicals that oxidize LDL cholesterol and attack the lining of your arteries.
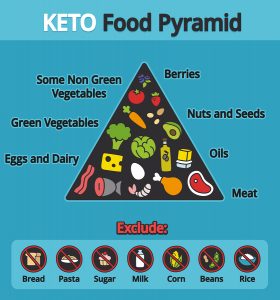
3. Cut out sugar and starchy foods
You need to cut out sugar and starchy foods because these will raise your LDL cholesterol and triglycerides, which also leads to hardening of your arteries. This is an important observation. Starchy foods are broken down by pancreatic juices into sugar, which enters your blood stream, causing an outpouring of insulin from the pancreas. When the short-term storage of sugar as glycogen is exhausted in muscle and liver tissue, the liver has to process any surplus of sugar that is still there. The end results are triglycerides and LDL cholesterol. Unfortunately the protective HDL cholesterol does not reach higher levels, when the LDL cholesterol is increased. A persistent diet of high-refined carbs will increase the risk for heart attacks and strokes. It follows from this that we are all better off cutting out sugar and starchy foods from our food intake.
4. Increase your soluble fiber intake
Increase your soluble fiber intake by eating vegetables, oats and oat bran, lentils, fruits and beans. Why does this decrease LDL cholesterol? The liver tries to eliminate too much cholesterol by binding it to bile salts and excreting it into your small bowel. But the last part of the small bowel reabsorbs some of these bile salts , and from there they return to the liver. This is called the enterohepatic pathway of bile salts. Soluble fiber intake binds those bile salts and prevents re-absorption in the enterohepatic pathway, eliminating cholesterol safely in stool. Soluble fiber from psyllium, pectin, beta-glucans and others have been shown in clinical trials to reduce LDL cholesterol by binding bile salts in the gut (interrupting the enterohepatic pathway).
Plant sterols and fiber supplements
Plant sterols (usually sold as sterol esters) are recognized by the FDA as reducing the risk of coronary heart disease, if taken in high enough amounts (2.4 grams of sterol esters per day). There are other useful supplements like artichoke extract, pomegranate, soy protein, Indian gooseberry (Amla), garlic and pantethine (vitamin B5) that are beneficial in terms of prevention of heart attacks and strokes. It would be too lengthy to get into more details here.
5. Take a whey protein supplement
There are two major milk proteins, whey and casein. Only whey protein binds to total and LDL cholesterol, lowering both. It is available in health food stores. Follow the package insert of the whey product for dosing.
6. Increase your omega-3 fatty acid intake
Omega-3 fats are healthy fats naturally present in fish oils and nuts. They increase the amount of circulating HDL cholesterol, which binds the bad LDL cholesterol. Go ahead and eat salmon, herring and mackerel as well as walnuts, ground flaxseeds and almonds. You can also take molecularly distilled (or pharmaceutically pure) EPA/DHA supplements. This pure form of fish oil is free of mercury and other heavy metals. EPA stands for eicosapentaenoic acid or omega-3 fatty acid. DHA is the acronym for docosahexaenoic acid, an important supplement for the brain. Tests have shown that fish oil supplements at a dosage of 3.35 grams per day of EPA plus DHA reduce triglycerides by up to 40%, equally to Lipitor or even more effective, but without the statin side effects. The end result is that your total cholesterol/HDL ratio decreases. This reduces the risk for heart attacks and strokes.
7. Eat foods with anthocyanin
In a 24-week study with diabetic people HDL levels rose by 19% when food was eaten that was rich in anthocyanin. This consisted of eggplant, purple corn, red cabbage, blueberries and blackberries. The advantage of raising the HDL cholesterol level is that the total cholesterol to HDL ratio decreases, which lowers the risk for heart attacks and strokes.
8. Exercising regularly
Exercising will increase your HDL cholesterol, which again decreases the ratio of total cholesterol to HDL cholesterol. This number should be between 1 and 3.5, the lower, the better.
9. Take a supplement called Ubiquinol, or Co-Q-10
Adults above the age of 60 need 400 mg once daily, younger people need between 200 mg and 300 mg daily. Co-Q-10 prevents oxidation of LDL cholesterol, which would aggressively attack the arterial walls causing hardening of the arteries. What causes oxidation of cholesterol? The answer is clear: fried foods like french fries or deep fried chicken will lead to oxidation; other culprits are margarine, commercially baked goods and cigarette smoking.
10. Calcium and vitamin D3
Recently a study on postmenopausal and overweight or obese women found that supplements of calcium combined with vitamin D3 lowered cholesterol.
11. Polyphenols
Flavonoids are the largest group among the polyphenols in such common foods as vegetables, fruits, tea, coffee, chocolate and wine. Over 130 studies on humans have shown improvement of the lining of the arteries (endothelial functioning) and lowering of blood pressure. Polyphenol consumption has a connection to a lower risk of mortality from heart attacks. Eat a Mediterranean type diet or a DASH diet, and you will automatically get enough polyphenols with your food. However, resveratrol, the powerful red wine polyphenol, warrants a separate daily supplementation as it prevents LDL oxidation in humans (Ref.1). Take about 250 mg of resveratrol daily.
12. Niacin/ nicotinic acid
This supplement comes as “flush-free niacin” and also as extended release niacin; it can raise the beneficial HDL cholesterol by 30 to 35% when patients take higher doses of 2.25 grams per day. In a metaanalysis of 7 studies researchers found a significant reduction of heart attacks and transient ischemic attacks (precursor syndrome before developing a stroke). Niacin can change the small particle LDL into a large particle size LDL, which is less dangerous. Niacin also reduces oxidation of LDL, which stops the atherosclerotic process. For a healthy person 500 mg per day of flush-free niacin is adequate.
13. Curcumin
This is a powerful heart and brain protector combining three different mechanisms in one; it is reducing oxidative stress, is an anti-inflammatory and counters the process that threatens to destroy the lining of the arteries. One study on healthy volunteers showed reduction of 33% in lipid oxidation, a 12% reduction of total cholesterol and an increase of 29% of the protective HDL cholesterol when patients took 500 mg of curcumin for only 7 days (Ref.1). This is the daily dose I would recommend for prevention of heart attacks and strokes.
14. Vitamin E (tocopherols)
This fat soluble vitamin is an antioxidant and in the past knew about its use as being heart supportive. Strangely enough some conservative physicians bad-mouthed this vitamin. In the meantime health practitioners have returned to using the vitamin. It turns out that there are 8 different types of tocopherols, with the alpha tocopherol being the best-known, but you also want to be sure that you are getting gamma tocopherol with your balanced vitamin E supplement every day. It remains the one that is a powerful anti-inflammatory. Simply ask staff at your health food store for a vitamin E supplement with gamma tocopherol in it. Take 400 IU per day (of the mix).
Conclusion
There is a lot you can do to control your cholesterol level by changing your diet, shedding some pounds, exercising and quitting smoking. All this will contribute to lower cholesterol. This will have a beneficial, long-term effect regarding prevention of heart attacks and strokes. In addition there are specific supplements and vitamins, which prevent heart attacks and strokes as well. With these measures the majority of people with high LDL cholesterol can change their cholesterol levels without taking statins. Statins have serious side effects like Alzheimer’s disease and a painful muscle condition called rhabdomyolysis. None of the other measures described here have any such side effect. Even if you chose to only concentrate on a few of these 14 points to lower cholesterol there will be significant improvements in your LDL and HDL cholesterol levels, when you ask your doctor to order these blood tests.
More info: https://www.askdrray.com/statins-can-hurt-the-consumer/
References
Ref. 1: Life Extension: Disease Prevention and Treatment, Fifth edition. 130 Evidence-Based Protocols to Combat the Diseases of Aging. © 2013