When people get diabetes or prediabetes, what foods lower insulin resistance? You may have heard that eating too many carbs and gaining weight can cause high insulin values. This causes the body’s insulin receptors to become sluggish, a condition called insulin resistance. Continuing to eat too many refined carbs leads to a critical point. You can suddenly run out of enough insulin and would develop type 2 diabetes at this time.
So, what foods lower insulin resistance?
Low glycemic food
Insulin resistance and type 2 diabetes occur because people do not pay attention to the glycemic load of the food they choose. Many people eat bread, pasta and starchy vegetables like potatoes. They also eat excessive sugary sweets, such as cupcakes, ice cream, or chocolate bars. All the pancreas can do is keeping blood sugar stable by overproducing insulin. But you can assist your pancreas to not overwork itself.
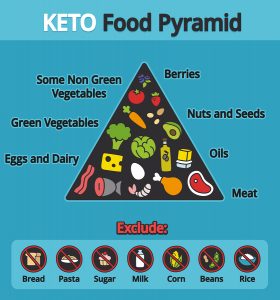
Leave the high glycemic index foods alone. Instead eat low glycemic foods like non-starchy vegetables (peppers, broccoli), lean meats, fish and nuts. Add high-fiber foods like beans and some whole grains. Eat foods rich in omega-3 fatty acids like salmon. Have a dessert with berries that are rich in antioxidants. Blueberries, strawberries, raspberries and black berries are all low glycemic foods, rich in vitamin C and antioxidants. They are “nature’s candy”.
Research on insulin resistance
In a study from Singapore differences of insulin sensitivity were found between lean Asian Indians and Chinese and Malays, living in Singapore. The Asian Indians had less insulin sensitivity, which means they had higher insulin resistance. This occurs because of a genetic variant of insulin sensitivity.
Another lengthy publication investigated the connection between metabolic syndrome and insulin resistance. In addition it examined the connection of heart attacks and strokes to wrong diets. The researchers pointed out that the percentage of diabetes and cardiovascular disease will reduce significantly on a sensible diet. How is this achievable? By adopting a healthy diet that also leads to weight loss.
Diets in the US and in the Western world have major shortfalls, due to the fact that people consume not enough vegetables, fruit and whole grains. Instead we see a higher intake of red and processed meat. In addition there was higher intake of sugar-sweetened foods and beverages. Refined grains and flour products are another unhealthy food source. In the US and other westernized countries we see an overconsumption of sodium and saturated fat.The key to a healthy diet was adopting a Mediterranean diet. A study exists where a group of patients with metabolic syndrome consumed mostly whole grains, vegetables, fruits, nuts, and olive oil. The control group simply followed a “prudent” diet.
What foods lower insulin resistance? The Mediterranean diet does!
Two years later the group on the Mediterranean diet showed the following results: they had a higher intake of monounsaturated fat (olive oil) and polyunsaturated fat (fish oil) and fiber. Their omega-6 to omega-3 ratio had decreased. The high-sensitivity C-reactive protein, a general measure for inflammation, had decreased. Other inflammatory kinins like interleukins had also decreased. The insulin sensitivity endothelial function score showed improvement. The important part overall was that the Mediterranean diet prevented the metabolic syndrome compared to the “prudent” control diet.
In 2018 a study from Spain was looking for positive effects when supplementing with olive oil or nuts. A Mediterranean diet with extra olive oil or extra nuts reduced the risk of heart attacks in a high-risk group compared to controls. The study included 7447 persons and these were the results after 4.8 years: the Mediterranean diet group that used more olive oil had 28% fewer cardiovascular events compared to the control group. The Mediterranean diet group with nuts had 31% less events. Heart attacks, strokes or death from cardiovascular disease were these “events”!
What foods are unhealthy?
In order to be able to avoid unhealthy foods it is important to identify what harms us. Foods to avoid are listed in this link. Sweetened beverages, fountain drinks, sodas and fruit juices contain loads of sugar. They will cause an insulin response and on the long-term insulin resistance. Avoid starchy vegetables, such as potatoes, pumpkin, corn, and yams. Also avoid processed snacks and boxed foods. Starchy foods break down into sugar, which also stimulates insulin release. Your no-food list continues with excessive sugary sweets, such as cupcakes, ice cream and chocolate bars. White bread, rice, pasta, and flour are also starchy, and the body breaks down starch into sugar and stimulates insulin production.
Some saturated fats are acceptable, but hydrogenated fat must be avoided altogether.
Epigenetic factors regarding insulin resistance
A recent publication on March 14, 2017 investigated the effect of exercise on insulin sensitivity in a mouse model where the mother mouse was obese.
Pregnant, obese mice were insulin resistant and the offspring came down with diabetes. But when the pregnant mice exercised, the insulin sensitivity came back to normal. In addition the offspring were not diabetic. This effect was not due to genetic factors. Instead the authors believe it was due to epigenetic factors, in this case treating insulin resistance with exercise. When the pregnant mother turns insulin sensitive, the offspring is programmed to regulate their blood sugar metabolism normally.
An April 2017 study from Korea investigated the effects of healthy nutrition on patients with metabolic syndrome and insulin resistance. They noted that avoiding unhealthy foods could normalize markers of disease.
The authors discuss how nutritional factors can contribute to inheritance of epigenetic markers in the next generation. They also showed how dietary bioactive compounds could modify epigenetic factors. Taking dietary components that regulate epigenetic factors contribute significantly to health. The authors concluded that a healthy diet could prevent pathological processes that otherwise would cause metabolic disease.
Conclusion
It is interesting to note that insulin resistance can be reversed into insulin sensitivity by eating healthy foods. Research papers are now describing how a healthy diet of the mother can affect her offspring positively. These effects are due to epigenetic factors, as genetic factors have not changed.
We are already hearing that diseases like heart attacks, high blood pressure, strokes, diabetes and others can largely be prevented by a proper diet. The key is to avoid high glycemic foods and eat low glycemic foods instead. It is not complicated. Eat non-starchy vegetables (leafy greens, peppers, broccoli), lean meats, fish and nuts. Add high-fiber foods like beans and some whole grains. Eat foods rich in omega-3 fatty acids like salmon. The end result is that insulin resistance disappears and metabolic processes return to normal. This was what Hippocrates had in mind when he stated “Let food be thy medicine and medicine be thy food.”