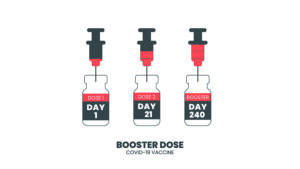
This article will inform you that booster vaccinations against Covid-19 variants are very effective. Studies in patients from Israel who received a third vaccination (booster shot) showed much less omicron infections. Researchers compared the number of omicron infections in patients with only two shots and another group with three vaccinations (regular vaccination+booster shot). In patients who had booster shots infection rates were 10-fold lower.
Antibody titers matter
What seems to be happening is that antibody titers against Covid-19 rise after each vaccination providing more and more protection against the virus. Patients in this study had 90% less Covid-19 infections after a booster (=3 shots with the Pfizer vaccine) when compared to a double vaccinated group. Researchers compared nursing home residents who were previously sick with Covid-19 versus those who were not. They did PCR tests in April or June of 2020 to identify that there was a past history of Covid-19 infection with a subsequent recovery. Within 3 weeks after one dosage of an anti Covid-19 vaccine their antibody tests rose to above 40,000 arbitrary units (AU) per milliliter. The threshold was 50 AU to be positive.
The Israeli experience
An Israeli study was published on Nov. 5, 2021. Researcher determined the antibody titers in blood samples after anti-Covid-19 vaccinations. They investigated the antibody titers after two vaccinations and compared them to antibody titers after three vaccinations. The latter vaccination is often referred to as a booster shot. 97 study participants had blood tests taken after two vaccinations with an average antibody titer of 440 AU/mL. Any value above 50 was considered to be seropositive. However, 10 to 19 days following the booster shot the average antibody titer rose to 25,468 AU/mL, which is an enormous increase.
Older age patients and kidney transplant patients responding to booster shots
After two vaccinations there were lower antibody titers in older patients aged 67-74 compared to patients age 18-55. But after the booster shot this age difference was no longer present. On the sideline the researcher also followed a group of kidney transplant patients. These would be considered to be patients with a chronic disease. Initially, following the standard two vaccinations these patients were negative for an antibody response. But after the third vaccination (booster shot) 49% of the kidney transplant patients showed a positive antibody test.
Antibody titers in patients with past natural Covid-19 infection
Researchers also investigated the antibody response of patients against the spike protein of Covid-19. A publication showed after a natural Covid-19 infection plus one vaccination of the Pfizer/Moderna vaccine the antibody titer was 20,120 arbitrary units per milliliter. In contrast, the other group consisted of two vaccinations of the Pfizer/Moderna vaccine. They had antibody titers of 22,639 arbitrary units per milliliter. This was not significantly different from the first group. It also did not matter whether in the first group the prior natural Covid-19 infection was 1, 2, 3 or more months before the first vaccination with the Pfizer vaccine.
Discussion
New information emerged since the beginning of the Covid-19 pandemic. There was confusion about how often people would need a vaccination before they would be immune against Covid-19. After one vaccination with the Pfizer/Moderna vaccine the protection rate against Covid-19 is around 50%. After two vaccinations the protection rate is around 95%. Experience with the booster vaccination teaches us that the protection rate is almost 100%. There was no difference between the antibody response of the group with the age of 18-55 and the group with the age of 67-74 after the third shot (booster shot).
But there is a proviso: the immune system must be capable of full activation to produce enough antibodies by the B cells. B cells are the lymphocytes that traveled through the bone marrow after which they started producing antibodies against viruses. As the results with the kidney transplant patients showed, only 49% of them were able to produce positive antibody titers. The reason for this is that kidney transplant patients must take immune system suppressing drugs to avoid a rejection of the kidney transplant.
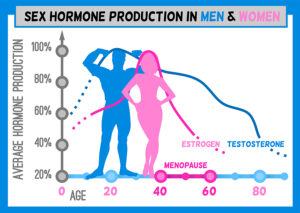
Other reason for poor antibody response
Other patients with chronic diseases (diabetics, autoimmune disease patients etc.) and patients older than 60 can also have a weaker immune system. Part of this can be when one or more of the 14 supplements is missing that are necessary for a full immune response. It is important before the Covid-19 vaccinations to take the 14 necessary supplements to get a good antibody response.
Conclusion
Several studies showed that the antibody response after the anti-Covid-19 vaccine increases significantly. The measurements revealed that after two injections the antibody titer was 440 AU/mL. After the third (booster) injection the antibody titer increased significantly to 25,468 AU/mL. This explains why some people after one or two vaccinations still may be able to come down with Covid-19, but after the additional booster injection (3rd vaccination) the immune response in terms of antibody production is 58-fold higher than after the second vaccination. This gives the immune system a full response. Some patients with chronic diseases (obesity, diabetes, autoimmune diseases etc.) will have certain immune deficiencies. This explains a higher infection rate among these people as well as a higher mortality rate. We all can take the booster vaccine against Covid-19. In addition, we can take the 14 immune supplements to stimulate our immune system.