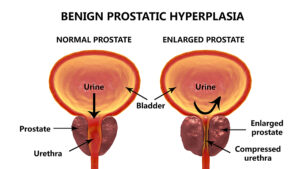
This article describes the use of green light laser treatment for an enlarged prostate. Physicians call an enlarged prostate “benign prostatic hyperplasia” or else “prostate hypertrophy”. When men turn older than 60, they often develop an enlarged prostate gland. This in turn can squeeze the urethra as it travels through the prostate resulting in problems passing urine.
A complication of an enlarged prostate gland can be frequent urinary tract infections
Men who have an enlarged prostate also often develop recurrent urinary tract infections. As a recent example that went through the news, former President Bill Clinton had to be hospitalized for such an infection. However, a simple surgical procedure like the green light laser treatment for an enlarged prostate allows for normal urination. This procedure opens up the previously narrowed urethra and reduces the prostate size to normal. As a result, the recurrent urinary tract infections stop. The green light laser treatment for an enlarged prostate is relatively new. It has much less blood loss than the conventional transurethral resection of the prostate (=TURP). The new laser procedure also goes under the name “green light laser TURP”.
History of the green light laser treatment for an enlarged prostate
In 2003 the first series of 10 patients with an enlarged prostate received treatment with a green light laser. After one year their prostate glands showed an average of 27% volume loss. This was less than 40-50% prostate volume loss with the conventional TURP procedure. In 2004 and 2005 urologists started larger series with the green light laser treatment were, also with a more powerful laser application. The urologists used 80 W instead of 60 W laser applicators. They achieved a reduction in prostate volume ranging from 37% to 53%. This was comparable to what conventional TURP treatments achieved.
Statistics regarding enlarged prostate glands
Prostate enlargement in older men is very common. By the age of 60 about 50% of men have an enlarged prostate gland. Compare this to men at 85 years: 90% of them have prostate gland enlargement. There is a lack of leadership among physicians regarding prostate hypertrophy. Many physicians consider it a minor nuisance in aging men. However, urinary tract infections that are rare in younger men are found more commonly in men with enlarged prostate glands. Also, urination problems can occur that may lead to bladder wall thickening and hydronephrosis of the kidneys. If no surgery is done for the prostate enlargement, the patient has to do intermittent or permanent urinary catheterization.
Surgical options for an enlarged prostate gland
TURP (transurethral resection of the prostate gland)
When patients have difficulties urinating or get frequent urinary tract infections, the urologist often recommends a TURP, which stands for “transurethral resection of the prostate gland”. This is the oldest form of prostatic surgery. The urologist introduces a resectoscope into the urethra and the prostate and removes bits and pieces of prostatic tissue. Complications can be bleeding, leakage of urine and infections after the TURP.
GreenLight™ laser treatment (Photoselective vaporization of the prostate)
This is a more modern form of the TURP, but the knife is replaced with a GreenLight™ laser. This procedure takes about one hour for most cases of prostatic hypertrophy. The urologist does a cystoscopy. When he views the prostate portion of the urethra a green light laser removes tissue from the prostate gland. This allows for free flow of urine through the urethra after the procedure. The advantage of this procedure is that the laser stops any bleeding right away, so patients lose only very little blood. More than 1 million GreenLight™ laser procedures have been performed around the world and urologists have done it on a large scale for about 15 years.
Water vapor therapy (Rezum™)
With this office-based procedure water vapor is introduced into the prostate gland, which causes some prostate tissue to die off. Over a 3 months period pieces of the prostate gland are shed into the urine. The urethra opens up and the prostate gland decreases in size. Unfortunately, many patients have to wear a urinary catheter for several days and sometimes weeks. Surgeons started to use this procedure on a large scale approximately 5 years ago and the urologist can do it at the office.
As the link shows, there are other treatments that urologists can do to open up the passage for urine and decrease the size of the prostate.
Best approach is the green light laser treatment for an enlarged prostate
Currently the best approach is the green light laser treatment for an enlarged prostate. The original TURP is too aggressive with bleeding complications after the procedure. The Rezum method has a prolonged recovery time and does not always succeed restoring normal urine flow. The green light laser treatment is safe, has a minimal amount of bleeding due to the nature of the laser and allows for a faster recovery. The green laser immediately stops any bleeding from the prostate gland.
Conclusion
Many older men beyond the age of 60 develop prostate gland enlargement. The prostate puts pressure on the portion of the urethra immediately underneath the bladder. This results in difficulties urinating and frequent urinations to empty the bladder. Often there are significant amounts of urine that stay in the bladder. This urinary retention predisposes the man to urinary tract infections. In the past urologists did transurethral resections of the prostate (TURPs). But they could be very bloody and in some cases caused leakage of urine or infections. 15 years ago surgeons started to use a new type of TURP, a green light laser treatment for an enlarged prostate. Green light laser stops any bleeding during the procedure right away. Post-surgical complications are minimal. Many urologists and patients prefer this method to treat prostate enlargements.