A review in CNN describes that irregular periods are linked to premature deaths. This review is based on the original publication in the British Medical Journal published on September 30, 2020.
Essentially, the researchers followed 79,505 premenopausal women without a history of cardiovascular disease, cancer, or diabetes for 24 years. The researchers recorded 1975 premature deaths. The definition for a premature death was someone dying before the age of 70. There were three age groups that the researchers followed separately for 24 years.
- ages 14-17 years
- 18-22 years
- 29-46 years
The most common causes of death were 894 from cancer and deaths from 172 strokes and heart attacks.
Death rates after 24 years for the three subclasses just mentioned
The researchers noted that there were differences in survival for different age groups. But there were also differences in survival for irregular periods versus prolonged intervals between periods. Crude mortality rates for 1000 person years of follow-up for women with normal versus irregular periods were as follows.
Normal periods Irregular periods
14-17 age : 1.05 14-17 age: 1.0
18-22 age: 1.23 18-22 age: 1.37
29-46 age: 1.0 29-46 age: 1.68
Women with a cycle length of 40 days or more had a higher mortality rate. The researchers compared this to women with a normal cycle length (26-31 days). Here are the data in detail for two age groups at the outset of the study.
Women with a cycle length of 40 days or more
Age 18-22: 1.34
Age 29-46: 1.40
Heart attacks and strokes followed these death statistics closest.
Discussion
The researchers concluded that teenagers and women in their middle-age were at the highest risk. This risk was for premature mortality, if they had irregular periods or a cycle length of 40 days or more. There was also an association between irregular periods and a prolonged cycle length and type 2 diabetes, ovarian cancer and coronary heart disease. In addition, mental health problems were also related, the study said.
Dr. Adam Balen, a professor of reproductive Medicine at Leeds Teaching Hospitals in the UK said: “Young women with irregular periods need a thorough assessment not only of their hormones and metabolism, but also of their lifestyle so that they can be advised about steps that they can take which might enhance their overall health”.
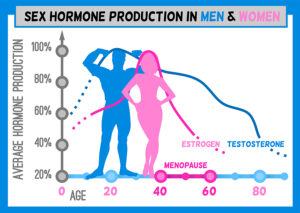
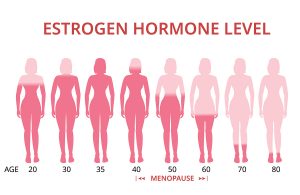
Too much estradiol in women and men can cause cancer
In this context it is interesting that other studies have shown that unopposed estradiol may be the culprit for both irregular periods and larger intervals between periods. When estrogen is elevated in females, irregular periods can result. Unopposed estradiol can cause breast, uterine and ovarian cancer.
In males who also have a small amount of estrogen in their blood, it is important that a larger amount of testosterone balances the two hormones. Otherwise there is a risk of prostate cancer.
In addition, cardiovascular disease has been described as a side effect of standard hormone replacement therapy (HRT) in women with synthetic hormones.
The good news is that treatment with bioidentical hormones can treat these abnormal periods. This eliminates premature mortality and in many cases prolongs life.
Conclusion
Researchers followed 79,505 premenopausal women without a history of cardiovascular disease, cancer, or diabetes for 24 years. They found that there is a linkage between irregular periods and premature deaths. There were three age groups that the researchers followed. Some of them suffered from irregular periods and others had periods that were 40 days or longer apart. The researchers recorded the premature mortalities. At an age of 29-46 there was a 68% higher mortality in women with irregular periods. The scientists compared this to women who had regular periods. In addition, women aged 29-46 with a cycle length of 40 days or more had a 40% higher mortality.
Estrogen dominance could explain premature deaths
The researchers compared this to women with a normal cycle length. It is possible that women who died prematurely were having too much estrogen in their system, which can produce cardiovascular disease and cancer of the breast, uterus and ovary. Further studies need to clarify the mechanism behind irregular periods and why a cycle length of 40 days or more causes mortality.