Several studies showed that new protein markers help diagnose cancer 7 years earlier than conventional tests. One study described how researchers were able to diagnose 19 different cancers years before other tests could show these results. Another study confirmed that 2,074 circulating proteins showed an association with 9 cancers. These consisted of bladder, breast, endometrium, head and neck, lung, ovary, pancreas, kidney, and malignant non-melanoma.
First study
The first study found 371 plasma protein markers that pointed to an increased cancer risk. 107 of them showed an association with cancers that physicians could only diagnose 7 years later. The researchers stated that there was an opportunity for early diagnosis and treatment. The treatment results would be much better than it is the case with a later diagnosis. In this study researchers examined plasma from 503,317 adults aged 39 to 73.
Second study
The second study found an association between 40 specific proteins and 9 common cancers as mentioned above. Researchers examined a total of 2,074 circulating proteins in 337,822 cancer cases. Of the 2074 circulating proteins only 40 proteins were specific for the nine cancers that I mentioned above.
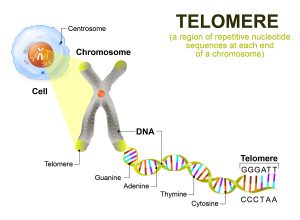
Proteomics
The scientists who performed the studies with data from the UK Biobank specialized in the discipline of proteomics. This involves a thorough investigation of proteins in blood plasma. Here is a summary of a discussion of the findings of both studies.
The first study identified plasma proteins that showed linkage to an increased risk of cancer of the liver, digestive and gastrointestinal tracts, non-Hodgkin lymphoma, as well as colorectal, lung, kidney, brain, stomach, esophagus, endometrium, and blood cancers.
The second study showed links of protein markers to these 9 cancers: bladder, triple-negative breast, endometrium, head and neck, lung, ovary, pancreas, kidney, and malignant non-melanoma.
The authors of both studies felt that their findings contributed to an early diagnosis of these cancers. Specifically, analysis of blood plasma proteins can diagnose cancer 7 years before a clinical diagnosis.
Discussion
Joshua Atkins, PhD, BBmedSci, a senior genomic epidemiologist at the University of Oxford stated: “Proteins that are not causal for cancer development, but are a consequence of cancer growth can provide avenues for detecting cancers at an earlier stage when treatment can be more successful.” Dr. Atkins said further: “Nevertheless, disruption of these processes can result in diseases including cancer. For some proteins, higher blood levels are linked to higher cancer risk, while others may be protective, so higher levels are linked to lower risk.” He explained further that protein concentrations are not always related to one tissue type. He said: “The protein FGFR3 is linked to an increased risk of bladder cancer, but lowering its levels is tied to an increased osteoarthritis risk.” It will take more investigations before a clinical test is available that physicians can order to diagnose cancer early.
Conclusion
Blood proteins showed linkage to a number of cancers in two separate research papers based on the UK Biobank data. The first study identified plasma proteins that were linked to an increased risk of cancer of the liver, digestive and gastrointestinal tracts, non-Hodgkin lymphoma, as well as colorectal cancer, also lung, kidney, brain, stomach, esophagus, endometrium, and blood cancers.
The second study showed links of protein markers to these 9 cancers: bladder, triple-negative breast, endometrium, head and neck, lung, ovary, pancreas, kidney, and malignant non-melanoma. On average these sensitive cancer tests can diagnose cancer 7 years before a clinician is able to diagnose it. In the future your doctor may screen you for cancer as you age, as cancer is mostly a disease of older people. Earlier diagnosis of cancer will give better treatment results.