Dr. Pamela Smith, an anti-aging physician gave a talk about what you must know about male hormones. She spoke on Saturday, Dec. 10, 2022 at the Sands Conference Center of the Palazzo Hotel in Las Vegas. The title was “What you must know about male hormones”. She presented 199 slides, so the following can only be a brief summary of what she said. She started by saying that the term “male menopause” goes back in time to 1944. Other terms are andropause and late onset hypogonadism.
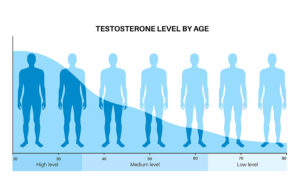
Different testosterone levels at different ages
It is important to realize that at age 20 the blood testosterone level is around 900 ng/dL, but this declines after age 30. It is 550 ng/dL at the age of 40. At the age of 50 the testosterone level is 350 ng/dL. And at the age of 70 the testosterone level has shrunk to 200 ng/dL or less. With this in mind, there are also seasonal variations with higher levels of testosterone occurring in summer and early fall, and low levels happening in winter and early spring. A healthy male produces the following male hormones: Testosterone, 5-6 mgs/day; Androstenedione, 3 mgs/day; DHT, 0.300 mgs/day; DHEAS, 50 mgs/day; and DHEA, 15 mgs/day.
Functions of testosterone
In other words, testosterone is the male hormone responsible for the male body characteristics. Every male body cell has testosterone receptors on it. Truly, this way testosterone is involved in protein manufacture and muscle maintenance. In fact, bone formation depends on testosterone and oxygen uptake as well. It is also controlling blood sugar together with insulin. In addition, normal sperm production depends on testosterone. To clarify, testosterone also regulates cholesterol and the immune system. By all means, it also helps to improve mood, is important for mental concentration and helps protect against Alzheimer’s disease. Finally, there is stimulation of platelets and megakaryocytes by testosterone, which makes blood clotting easier.
Symptoms of andropause
It must be remembered, towards the end of their 60’s many men get symptoms of tiredness, loss of energy and depression. Specifically, they may get a bad temper, present with irritability, anxiety and nervousness. Specifically, they complain of a loss of memory, loss of sex drive and libido. Certainly, their erections are getting weak or they lose them altogether. There is a decreased intensity of orgasm and they are gaining weight. All this should prompt their physician to have a total testosterone blood test done. When the testosterone level is less than 500 ng/dL the person should see their physician for replacement testosterone therapy.
Other signs of testosterone deficiency
There are other signs and symptoms of testosterone deficiency: backaches and joint pains, loss of fitness, being overstressed. In addition, testosterone-deficient males experience a decrease in job performance and a decline in physical fitness. They have bone loss, elevation of their blood cholesterol and an increased risk of heart disease. They often also have increased insulin resistance, diabetes and metabolic syndrome. Mortality in men with low testosterone is much higher than in controls with normal testosterone. Several dozens of literature references were provided to support the above statements.
Testosterone replacement and hormone balance
When a patient is on testosterone replacement, a digital rectal exam should be performed to check for the size of the prostate gland. A PSA should be done every year (in former prostate cancer patients every 3 months). PSA should stay below 4.0 ng/mL. If the PSA rises by 1.5 ng/mL in one year or by 0.75 ng/mL in two consecutive years, a urologist should be consulted to rule out prostate cancer.
Men produce small amounts of estrogens, which are important for memory function of the brain and for strong bones. Androgens and testosterone aromatize into estrogen via the enzyme aromatase in fatty tissue. There are a few reasons why aromatase increases: obesity, excessive alcohol intake, chronic inflammation and high insulin levels.
The following medications lower estrogen levels: phenobarbital, carbamepazine, trazodone, chlordiazepoxide and sulcrafate.
Side effects from elevated estrogen levels
Increased estrogen levels in males cause gynecomastia (colloquially called “beer tits”), decreased sex drive, heart attacks, strokes and benign prostate hypertrophy. Elevated estrogen levels also cause insulin resistance, rheumatoid arthritis and prostate cancer. Dr. Smith referenced all of these statements again with many literature quotations.
Dihydrotestosterone (DHT)
This metabolite of testosterone is 3-times stronger than testosterone. It is formed from testosterone by the enzyme 5-alpha reductase. It is responsible for the male-specific characteristics, the male genitalia and the prostate gland. Low levels of DHT cause reduced sexual function, decreased libido and weakened muscle function. On the other hand, elevated DHT causes male pattern baldness, hirsutism and benign prostate hypertrophy (BPH). There are two 5-alpha reductase inhibitors, namely finasteride and dutasteride, that clinicians use to lower elevated DHT levels. This can reduce the risk of prostate cancer by about 50%. Dr. Smith provided many literature quotations to support these statements.
Testosterone replacement therapy
Based on more than 3 dozen literature quotations Dr. Pamela Smith outlined the following:
- Most men tolerated transdermal testosterone application very well.
- Erectile dysfunction affects 1 in 5 older men.
- Erectile dysfunction in association with low blood testosterone and low libido responds to transdermal application of testosterone very effectively.
- It may take 14-25 weeks before transdermal testosterone treats erectile dysfunction successfully, more than 50% of men respond to this.
- Testosterone replacement prevents beta amyloid precursor protein production, which increases memory and decreases the risk of Alzheimer’s development.
- High stress produces high cortisol levels in the blood, which affect the hippocampus, where memory is located. Testosterone is neuroprotective, and it preserves memory.
- Transdermal testosterone decreases coronary heart disease by relaxing coronary arteries. This prevents heart attacks and strokes.
- Testosterone decreases inflammation and lowers LDL cholesterol.
More facts about testosterone replacement therapy
- Testosterone lowers inflammatory cytokines and stimulates interleukin-10 production. This has anti-inflammatory and anti-atherogenic actions, which prevents heart attacks.
- There was a reduction in mortality from heart attacks in the testosterone treated group of between 66% and 92%. In addition, 30 nonfatal strokes and 26 nonfatal myocardial infarctions occurred in the control group, but none in the testosterone group. Testosterone deficient heart failure patients responded very well to testosterone replacement therapy.
- Prostate cancer or benign prostate hypertrophy do not increase with transdermal testosterone replacement therapy.
- A Meta-analysis showed that older men with the highest risk for prostate cancer have the lowest testosterone blood levels.
- Type 2 diabetics with a high insulin resistance respond well to testosterone replacement therapy. They increase insulin sensitivity and lower their blood sugars. This improvement peaks after 3 months and the effect stays for 12 months.
Further facts about testosterone replacement therapy
- Testosterone replacement is safe. It provides significant benefits for erectile dysfunction, for muscle mass, prevention of Alzheimer’s disease, prevention of heart attacks and strokes. Testosterone treatment is for males above the age of 50, there is no cut-off for higher ages. There are many controlled clinical trials spanning over 70 years, which support all of what is presented here.
- Testosterone can’t be taken orally, because it is rapidly metabolized in the liver. Instead, patients use transdermal testosterone gel or cream. Gels are commercially available and very expensive. Compounding pharmacies can provide testosterone creams for you, which are considerably cheaper and can be dosaged according to the patient’s needs. Testosterone esters in oil are available for subcutaneous or intramuscular injection twice per week. This ensured a steady testosterone level.
Improvements after testosterone replacement therapy
- Timing of improvements: cholesterol reduction occurs by 12 months, for triglycerides it takes 22 months. Testosterone levels take 4 to 12 weeks to normalize. Fasting blood sugars and Hemoglobin A1C come own within 3 months with further improvements by 12 months. Sexual desire and energy are back to normal within 3 to 6 weeks.
- It is important that you go for blood tests to measure testosterone levels every 3 months initially (blood level). If the levels are stable, the physician may decide to only order tests every 6 months.
Conclusion
The goal in the aging male is to maintain optimal male hormone levels. This achieves optimal health and prevents diseases of older age. First, it is important to preserve his erections, but at the same time testosterone replacement therapy prevents Alzheimer’s disease and memory loss. It also prevents heart attacks and strokes. Testosterone helps to preserve muscle mass. Hormone replacement therapy keeps lipids like cholesterol and triglycerides under control. Testosterone replacement reduces blood sugars and prevents type 2 diabetes mellitus. Replacement therapy also reduces elevated insulin levels. The end result is that testosterone replacement therapy maintains the health of the aging male.