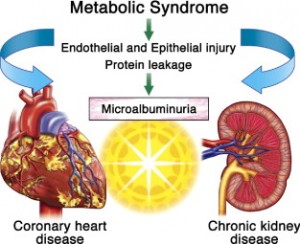
The metabolic syndrome is a new disease entity that is known to be associated with obesity. In order to make the diagnosis of metabolic syndrome at least 3 of the 5 components listed in the table under this link (hypertension, hypertriglyceridemia, low high-density lipoprotein cholesterol level or LDL cholesterol, high glucose level, abdominal obesity) have to be present.
Dr. Jing Chen and colleagues of Tulane University School of Medicine in New Orleans, La., published an analysis of the Third National Health and Nutrition Examination Survey in the Feb.3, 2004 edition of the Annals of Medicine. Patients with chronic kidney disease were identified in this study where 3, 4 or 5 of the metabolic syndrome criteria were positive. Two criteria for chronic kidney disease were measured:
1. if there was a significant reduction of the filtration capacity of the kidney.
2. if there was critical leakage of blood protein into the urine.
Depending on how advanced the metabolic syndrome was (all 5 criteria of metabolic syndrome positive versus only 3 or 4) there was a higher or lower risk of developing chronic kidney disease.
I have depicted the results of this study in bar graph form here. It shows clearly that chronic kidney damage occurs in a dose-response curve pattern depending on how severe the degree of the metabolic syndrome is.
| Risk of developing kidney disease with various degrees of severity of the metabolic syndrome |
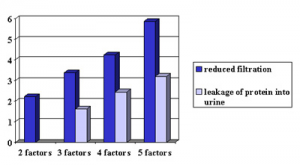 |
With 5 factors of the metabolic syndrome present the risk to develop reduction in filtration capacity of the kidneys is almost 6-fold. This is 3-fold higher than in a person with a milder degree of metabolic syndrome where only two factors are present. Such a person would only have a 2-fold risk for developing chronic kidney damage (dark blue shaded bars in graph). A dipstick urine test can measure protein in urine, which is an alternative way to measure kidney damage due to the metabolic syndrome. These values followed a very similar dose-response curve (light blue shaded bars in graph). The authors of this study believe that the kidney damage inflicted by the metabolic syndrome is different from that caused by high blood pressure or by diabetes. Future studies will have to establish whether this type of kidney damage can be repaired by treating the metabolic syndrome with a low glycemic, calorie restricted diet coupled with exercise.
Based on an article published in: Ann Intern Med 2004:140:167-174.
Last edited December 8, 2012