Introduction
In the June 21, 2007 issue of the New England Journal of Medicine a randomized study of 8.7 year duration the question was examined whether postmenopausal women following hysterectomy would have a higher risk with estrogen replacement therapy than controls who did not take estrogen therapy. The lead author was Dr. JoAnn E. Manson of Harvard Medical School and the method chosen to examine the heart disease risk was a CT of the heart to measure calcium in plaque of coronary arteries.
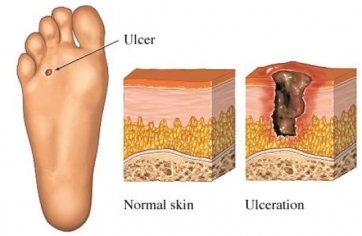
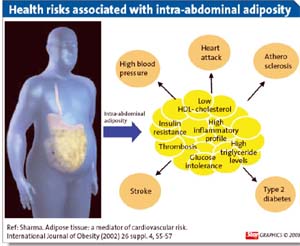
Previous research had shown a good correlation of calcification of coronary arteries with the degree of hardening of coronary arteries as shown in this image.
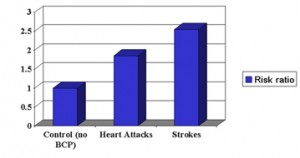
Various doses of estrogen were used and overall there was a reduction of calcium scores in all of the groups ranging from 22% to 31% when the calcium scores of the estrogen treated patients were compared to the non treated controls. This translated into 36% to 64% less heart attack rates when the treated groups were compared to the controls not treated with estrogen.
Discussion regarding estrogen replacement therapy
The discussion regarding estrogen replacement therapy following menopause is not finished, but women can be reassured that the cardiovascular risk appears to not be as straight forward as research seemed to suggest in the recent past. There likely was a bias in these retrospective studies and the present prospective study is much stronger having been done over 8.7 years following randomization. As this study was done on patients who had previous hysterectomies, there is no concern about uterine cancer. Breast cancer risk was not examined in this study.
The authors concluded that low dose estrogen replacement with 0.625mg of conjugated estrogen (Premarin) appears to be safe and has the most beneficial effect on coronary artery health when taken between the ages of 50 and 59. However, the authors also cautioned that estrogen would have multiple effects and may have negative effects on the cardiovascular system in some other way.
Reference: N Engl. J Med. 2007;356:2591-2602
Comment
Comment on Nov. 18, 2012: The real problem of this study is that the authors took the wrong “hormone replacement”, namely Premarin, which is a non-bioidentical estrogen concoction from horses, which translates into an ill fitting key. The human body’s estrogen receptors do not fit this “key”. The proper experimental set-up would have been to use bio-identical estrogen hormones, which are usually given as a cream and would be the perfect key for the human estrogen receptors. This would have to be balanced with bio-identical progesterone to achieve a balance the way it is in a younger woman. We know from other studies that this prolongs life by preventing coronary artery disease, prevents Alzheimer’s disease, prevents strokes and does not cause uterine cancer or breast cancer. Women on bio-identical hormone replacement also retain their normal sex drive.
See this chapter on menopause in the Net Health Book.