It seems like conventional medicine has ignored for several decades that lower blood sugar prevents diabetes. Medical researchers reevaluated the normal range for blood sugar and hemoglobin A1C, which is a 3 months average of blood sugar values.
In 2016 UCLA researchers reported that 46% of adults in California are either prediabetic or have diabetes.
In contrast 33% of young adults (age 18 to 39) also have prediabetes.
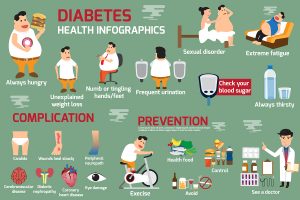
What is worse is the fact that even patients with prediabetes get complications. Normally only patients with diabetes suffer from these. These include kidney disease, retinal problems with loss of vision, neuropathy, hardening of the arteries and cancer.
Key to preventing this from happening is to recognize that prediabetes is already the beginning of diabetes. Not only is it important to prevent diabetes, but prediabetes as well.
Determination of prediabetes and diabetes
The conventional test for diabetes is a fasting blood sugar.
Prediabetes
In the past there was a consensus that patients with prediabetes had a fasting blood sugar between 100 and 125 mg/dL (5.6 to 6.9 mmol/L).
Diabetes
126 mg/dL (7 mmol/L) or higher on two separate tests indicates that you have diabetes.
Glycated hemoglobin (A1C) test
This test gives an average of blood sugar over 2 to 3 months. Physicians thought that a hemoglobin A1C test below 5.7% would be normal, between 5.7 and 6.4 percent they considered it to be prediabetes and at 6.5 or higher on two separate tests meant a diagnosis of diabetes.
Re-evaluating normal ranges to diagnose diabetes and prediabetes
Many researchers have said that the normal values from the guidelines for blood sugar or for glycated hemoglobin A1C are too high. This is the reason why diabetic complications developed even with prediabetes.
At the 22nd Annual World Congress on Anti-Aging Medicine In Las Vegas (Dec. 10-14, 2014) Dr. Piliszek stated that the normal range for hemoglobin A1C is skewed in the medical literature. It should be: 3.8% to 4.9%. This is very important to know for diabetics and any caregiver who looks after diabetes patients. If you consider a hemoglobin A1C of 6.0 as “normal”, the diabetic patient has the risk of dying prematurely of a heart attack or a stroke. According to the new guidelines even a patient whose hemoglobin A1C is 5.5 has diabetes and needs aggressive treatment to prevent complications associated with diabetes. Conventional guidelines would have considered this patient to be normal.
A 1999 study made it clear that patients with a blood sugar of more than 85 mg/dL were at risk of developing diabetes complications. Researchers observed about 2000 patients with fasting blood sugars of more than 85 mg/dL over 22 years. About 40% of them died of heart attacks or strokes! Because of studies like this, physicians demanded the new diabetes guidelines.
The authors concluded that fasting blood glucose in the upper normal range was an independent risk factor of cardiovascular death.
New guidelines
Prediabetes is not a separate diagnosis, but is mild early diabetes, which is reversible with aggressive treatment. Dietary changes (cutting out sugar and refined carbs) are often effective. In some cases the addition of metformin may be required.
The new normal ranges are:
Fasting blood sugar of 85 mg/dL or less is normal.
Hemoglobin A1C of 3.8% to 4.9% is the new normal range.
These values are based on observing patients over a long period of time and seeing whether or not they develop complications from diabetes.
Most noteworthy, uncontrolled diabetes leads to complications like damage to the lining of the arteries in all the key organs. It is the cause for the following conditions: kidney damage (nephropathy), eye damage (retinopathy), brain and nerve damage (neuropathy), as well as heart attacks and strokes (vascular damage).
Certainly, patients often end up with dialysis when kidney failure has set in. Retinopathy causes blindness and neuropathy leads to excruciating pain. Heart attacks and strokes often cause premature death. Those who ingest a high-glycemic diet have a 49% higher risk of getting lung cancer than those with a low-glycemic diet as this link from the MD Anderson Cancer Center showed.
Calorie restriction
A research group found that calorie restriction reduced fasting insulin levels in a group of overweight men and women.
Another study showed that restrained eating patterns lower fasting glucose and postprandial (after meals) glucose. As a result it also improved insulin sensitivity in normal weight individuals.
Some practical hints about diets to treat diabetes
- First of all, the obvious fact is that excessive sugar intake is harmful. But in addition a drastic reduction of refined carbs is also needed, as they just turn into sugar within half an hour of ingesting them. Cut out potatoes, pasta, and bread. You may have a slice of rye bread or full grain bread occasionally. This type of diet is called a low-glycemic index diet. Hence, as indicated earlier a study from the MD Anderson Cancer Center has shown that lung cancer is more common the higher the glycemic index is and is also more common in diabetics.
- Also, a Mediterranean diet has been shown to be anti-inflammatory. As diabetes and prediabetes are associated with chronic inflammation, it is useful to go on a diet that counters inflammation. Similarly, the DASH diet, which was developed for high blood pressure patients, is also anti-inflammatory. Here are a few examples of snacks that may be helpful.
- Finally, include fish and fish oil supplements in your diet. These contain omega-3 fatty acids, which are anti-inflammatory. Another useful piece of advice: eat lots of vegetables and salads as they contain healthy bioflavonoids and antioxidant vitamins. This stabilizes the lining of your arteries.
Conclusion
The old blood sugar and hemoglobin A1C guidelines need a significant revision. In contrast, new guidelines based on actual measurements and clinical trials that showed no complications of prediabetes on the long term have replaced them.
A fasting blood sugar of 85 mg/dL or less is normal. A hemoglobin A1C of 3.8% to 4.9% is now the new normal range.
Consequently, the doctor needs to be more aggressive about early nutritional intervention and probably include metformin as well to restore insulin sensitivity. It is no longer appropriate to allow complications of diabetes like nephropathy, retinopathy or neuropathy to develop. Unfortunately food manufacturers still overload processed food with sugar. Each patient needs to be vigilant about the food he/she eats. Therefore, low glycemic nutrition is the mantra to follow. Also stick to natural, unprocessed foods instead of the highly processed foods that populate the shelves of the supermarkets.