We are asking ourselves: When is someone at risk for suicide? This year’s National Suicide Week was from Sept. 4 through 10, 2022. Every day of each year it is important to be aware of signs and symptoms of impending suicide. However, the purpose of the yearly National Suicide Week is to really bring it to everyone’s attention how common deaths by suicides are. We all can contribute to improve the situation by increasing our awareness.
Some suicide statistics
In the US alone nearly 46,000 persons died by suicide in 2020. This means that there is one death by suicide every 11 minutes. In 2020 nearly 800,000 died by suicide worldwide. About 1.2 million attempted it. The hope is that the public will learn through education to recognize the signs of an impending suicide. This way the suicidal person can get counselling and hopefully not commit suicide.
Abnormal behaviors to watch out for
People who are getting suicidal may practice with guns, overdosing with pills or handle potentially lethal items. Other behavioral red flags could be giving away cherished items. The suicidal person may sleep too much or not enough. Isolation or withdrawal may be another pointer in a previously sociable person that he or she is becoming suicidal. Revenge thinking, reckless driving, agitation can all be pointers as well that the person is preparing for suicide. Justin Baker is the clinical director of The Suicide and Trauma Reduction Initiative for Veterans at The Ohio State University Wexner Medical Center. He said: ”A lot of times people need to kind of work up to that actual making an attempt because it’s a biologic thing you have to go against, your own survival”.
Watch what people say
When people become suicidal their words often indicate what they want to do. It is a warning sign, if someone is talking about wanting to die, by suicide or otherwise. Some people state that they feel like they have no reason to live. This is an alarm signal that they may be suicidal. Some people say that they feel like they are a burden for the people living around them. Other problematic statements are: “You don’t need me for this anymore” or “I feel like it’d be better if I just wasn’t here.” Someone uttering statements like these should get counseling. This allows them to vent their feelings and to reassess their situation.
Suicide risk factors
Hopelessness: People may express that they feel the future won’t be any better. Or they do not see a way out of the pain that they are in.
Obsession with death and dying: Some people ruminate about dying and they develop a plan what they may want to do to themselves.
Extreme mood swings: When somebody who usually is depressed and stressed behaves calm or cheery, this is an alarm sign that the person may be suicidal. They may have struggled with their decision to kill themselves, but when they accepted that this is what they want to do it calms their mind.
Past trauma: Abuse, trauma and neglect in the past are risk factors for suicide in the future.
Drug abuse: substance abuse predisposes a person towards being suicidal later on in life.
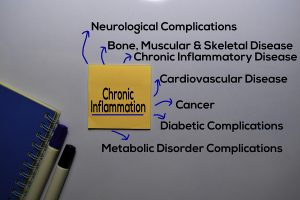
More suicide risk factors
Severe chronic illness with chronic pain: when a person has a chronic illness, and it is difficult to treat, people lose hope and they feel trapped. At this point suicide appears to be an option.
Mental disorders: people with schizophrenia, anxiety, depression or personality disorders are at a higher risk to turn suicidal. This is particularly so when they did not receive treatment and their mental condition deteriorates.
Family history, other factors and teen suicides
Family history of suicide: when there is a family history of suicide or a personal history of failed attempt of suicides the risk of suicide is much bigger than in the general population.
Other factors: There are many more factors that all can have a bearing on the risk for suicide. Financial loss and loss of a job are examples, but also prolonged stress from bullying or harassment. Divorce, breakup of a relationship, insufficient social support and many other negative emotions can contribute to a risk for suicide as well. A lot depends on the emotional make-up and the resilience of a person.
Teens: Teens are particularly vulnerable to commit suicide. It is important to listen to the teen in trouble and to arrange for counseling and support. More on teen suicide here.
What to do when faced with a person who contemplates suicide?
There are several crisis phones that are important to remember. In 2019 congress in the US has proposed to establish crisis lines with a simple 3-digit number: 988. But not all states have this number activated yet. The national crisis line in the US is: 1-800-273-TALK (1-800-273-8255).
In Canada the crisis hotline is: 1-833-456-4566.
There are counselors who have experience in listening to people in distress and talk to them.
When a person wants to commit suicide call 911. Sometimes a person in mental distress needs to be hospitalized and treated by a psychiatrist. Some people may benefit from electroconvulsive therapy, others from antidepressants. Cognitive therapy and behavioral therapy have a place as well in treating depressed patients. Close follow-up is important to prevent a relapse.
Conclusion
This year’s National Suicide Week was from Sept. 4 through 10, 2022. In the US alone nearly 46,000 persons died by suicide in 2020, nearly 800,000 died by suicide worldwide. It is important to recognize the signs of impending suicide. There are several high-risk factors that point to impending suicide, such as hopelessness, obsession with death and dying and extreme mood swings. There are certain constellations that are associated with a high risk for suicide: a history of a mental disorder, a break-up of a relationship, a severe illness with chronic pain and others. It is important to get the person at risk to a counselor or psychiatrist.
Treatment intervention for suicidal person
By talking it out, the pain of suffering gets eased. If there is an underlying depression it can be treated with various treatment modalities. Cognitive behavior therapy may help to change the negative thought patterns. It is important to intervene early. Close follow-up to prevent a relapse is also important.