Notably, there are health benefits from vitamin C supplements as I will explain below. A recent publication in the Journal of Intensive Care stated that vitamin C may lower ventilator time for sick patients in the ICU. In this case, researchers performed a meta-regression analysis. It is important to realize that higher doses of vitamin C changed the need for ventilation. Vitamin C given intravenously or by mouth significantly reduced the need for ventilation in sick patients. To explain, the researchers pooled eight clinical trials and compared them to a control group who did not receive vitamin C treatment. In detail, the researchers noted that there was a 14% reduction with regard to ventilator use in the treatment group. To clarify, they had received vitamin C infusions while patients who did not receive vitamin C infusions served as controls.
Five of the clinical trials involved patients who received 10 hours or more ventilation treatment. Certainly, these patients were sicker than the average ICU patients. They experienced a 25% reduction of ventilator time after receiving between 1 and 6 grams of vitamin C. The physicians gave this intravenous or orally.
History of Mega doses of vitamin C
Indeed, in the 1940’s mega doses of vitamin C were given intravenously in an attempt to treat polio. Eventually, in the late 1960’s Linus Pauling called high doses of vitamin C the “healing factors for diseases”. But subsequent clinical investigations showed that vitamin C had limitations. The Oregon State University website reports that some of the claims about vitamin C in the past went overboard. Here are some points about vitamin C that we need to remember.
- Vitamin C is an important cofactor in many enzymatic reactions, such as the biosynthesis of collagen, carnitine and neuropeptides. In addition, the regulation of gene expression requires vitamin C and vitamin C is an important antioxidant.
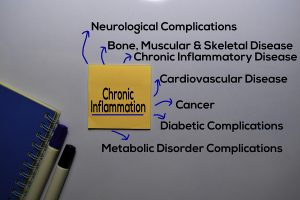
- A prospective cohort study showed that higher vitamin C blood levels lowered the risk of high blood pressure, coronary heart disease and strokes.
More effects of vitamin C
- Patients in need of a surgical procedure benefitted from vitamin C. Researchers showed that vitamin C was a valuable adjunct to conventional medicine in cardiovascular disease Vitamin C reduced arrhythmia and myocardial injury following cardiac procedures.
- There is insufficient evidence that regular vitamin C intake prevents cancer. Randomized controlled clinical trials reported no effect of vitamin C on cancer.
- 10 grams per day of vitamin C has no association with toxic or adverse effects in most people. However, some adults are more sensitive to vitamin C and develop gastrointestinal disturbances and diarrhea with megadoses of vitamin C. For these people physicians recommend taking up to 2 grams per day of vitamin C.
Vitamin C and disease prevention
Several clinical trials involving vitamin C supplements showed significant positive effects on patients. Below I am briefly reviewing these clinical trials.
Endothelial function
Endothelial function was improved with doses of above 500 mg of vitamin C. This likely is the reason that there is a reduction of cardiovascular disease in people who consume 1000 mg of vitamin C daily.
High blood pressure
Vitamin C at 500 mg daily lowers high blood pressure. A clinical trial found that 500 mg of vitamin C daily lowers the systolic blood pressure by 3.84 mm mercury and the diastolic blood pressure by 1.48 mm mercury. Over several years’ time this can prevent premature heart attacks and strokes.
Vitamin C and the immune system
Vitamin C is a powerful antioxidant. It can neutralize reactive oxygen species, which are produced when the immune cells fight viruses and bacteria. Neutrophils, lymphocytes and phagocytes are all supported by vitamin C. Vitamin C and E co-operate in their antioxidant functions. Vitamin C is essential for a strong antibody response with bacterial or viral infections. I take 1000 mg of vitamin C once daily.
Heart failure, strokes and heart attacks
Many studies showed some effects on reduction of heart attacks, strokes and congestive heart failure. With respect to strokes there was a 42% risk reduction over 9.5 years when the highest vitamin C plasma level was compared to the lowest level. But results regarding heart attack prevention and prevention of CHF were only marginal.
Cancer and vitamin C
Stomach cancer: there was a 45% reduction of stomach cancer when high vitamin C plasma level cases were compared to low plasma level cases.
Colon cancer: A pooled study based on 13 prospective cohort studies showed that vitamin C supplementation reduced colon cancer risk by 19%.
Large B cell lymphoma: After 11 years of follow-up the Women’s Health Initiative found that vitamin C supplementation reduced diffuse large B cell lymphoma by 31%.
Researchers could not show significant effects of vitamin C on other cancers.
Type 2 Diabetes (=adult onset diabetes)
A large European study going on for 12 years showed a strong inverse relationship between blood levels of vitamin C and the onset of diabetes. Patients with the highest vitamin C blood levels had a 62% lower risk of developing diabetes. Physicians compared this to low level vitamin C controls.
Mortality reduction with vitamin C supplementation
In the EPIC-Norfolk prospective study a clear inverse relationship was found with higher vitamin C blood levels and a reduction in risk of all-cause mortality.
Recommended dietary allowance for vitamin C
The official dietary recommendation for vitamin C in adults is 90 mg daily for males and 75 mg daily for females. However, in view of the above mentioned clinical trials I would recommend the following. Supplement with 500 mg to 1000 mg of vitamin C daily to have enough vitamin C reserves. The reason I say this is that the official dietary recommendation was based on preventing scurvy, the historic insufficiency disease of vitamin C. In addition, as mentioned before, vitamin C is safe to take up to 10 grams per day. Many physicians recommend taking a smaller amount of vitamin C found to prevent strokes, high blood pressure, type 2 diabetes, improve endothelial function and strengthen the immune system.
Conclusion
In my review I discussed health benefits from vitamin C supplements. Briefly, doctors noted that severely sick patients on respirators in the ICU setting were able to reduce the ventilator use. This was significant after they received between 1 and 6 grams of intravenous or oral vitamin C. However, patients with the highest vitamin C supplementation had a 62% lower risk of developing diabetes than low level vitamin C controls. Vitamin C lowered high blood pressure moderately and prevented strokes by 42%. Vitamin C stimulates the immune system together with vitamin D, A, E and some trace minerals. There are many more health benefits from vitamin C supplements. The official dietary recommendation for vitamin C in adults is 90 mg daily for males and 75 mg daily for females. However, I take 1000 mg of vitamin C daily as the evidence shows that this is healthier.