Dr. Flavio A. Cadegiani gave a talk saying that weight loss surgery is unnecessary. Dr. Cadegiani is the director of a weight loss clinic with the name Corpometria Institute in Brasilia, Brazil. He is board certified in endocrinology and metabolism and in internal medicine. He presented his talk at the 24th Annual World Congress on Anti-Aging Medicine (Dec. 9-11, 2016) in Las Vegas that I attended.
Here are the main topics that he presented.
Weight measurements are wrong when based on the BMI
Dr. Cadegiani stated that we do not understand obesity, because we look at it from the wrong angle. Current dietary approaches have failed. But obesity research is still proceeding in the wrong way. If all else fails, weight loss surgery is finally the last resort. But this is wrong.
The problem with body mass index (BMI) is that people would consider an athletic body type “obese”, because the BMI exceeds 30.0. However in a very muscular person the reason for the elevated BMI is an increased muscles mass, not fat. Body composition scales reveal that, but a simple weight measurement does not.
Dr. Cadegiani recommended measuring waist circumference with <94 cm (37 inches) for men and <88 cm (34.65 inches) for women being normal.
10 reasons why we are misled by the BMI
- The inventor of the BMI was a mathematician. He explicitly stated that the BMI would not predict the level of fatness of an individual. The other factors are bone mass and muscle mass.
- Because the BMI ignores the waist size, it is scientifically invalid.
- There are physiological reasons why it is wrong: studies did not factor in the relative proportion of the bone, muscle and fat content.
- The BMI gets the logic wrong: the CDC site claims that the BMI “is a reliable indicator of body fatness for people”. This is simply not true!
- The BMI is based on bad mathematics: the formula assumes low muscle mass and high fat content.
- The BMI is lying by scientific authority: Dr. Cadegiani said it has an “air of scientific authority, but it is mathematical snake oil.”
- The BMI suggests that there are distinct categories of underweight, ideal, overweight and obese. It assumes sharp boundaries that hinge on a decimal place. All of this is nonsense.
- Cynical people could suspect that medical insurance companies lobby for the continued use of the BMI as it keeps their profits high. Sometimes insurance companies charge higher fees for people with an elevated BMI.
- Doctors can contribute to the continued use of the BMI, if they don’t feel the need to use another way of assessing their obese patients.
- It is embarrassing that we still base the assessment of obesity on a 200-year-old mathematical formula when we know of more reliable measures.
Bariatric surgery done too easily
Dr. Cadegiani noted that publications on bariatric surgery (=weight loss surgery)
underreport surgical complications and deaths. The bariatric industry is rich, and 90% of the booths during obesity conferences belong to bariatric-related companies. Long-term follow-up studies are lacking. Those who do follow-ups report an increase of pancreatic tumors after 10 years following bariatric surgery.
Long-term follow-ups also describe a 70% increase of psychiatric disorders including depression and alcoholism. Those who had bariatric surgery experience a 200% increase in suicides.
Overcoming weight centered approach
Here is how to avoid the weight-centered approach that would lead the clinician to wrong conclusions.
There are four factors that need consideration:
- The assessment includes metabolic blood markers
- The assessment incorporates body composition scales
- The patient participates by measuring waist circumference and body weight
- The clinician incorporates clinical signs and symptoms
Classic metabolic markers are liver enzymes and hormone levels like testosterone, Thyroid (T3) LH and IGF-1. Apo B and triglyceride levels have to come into consideration for a lipid metabolism assessment. The physician monitors inflammation through a combination of uric acid levels, ferritin and C-reactive protein (CRP). An oral glucose tolerance test and fasting insulin level can predict diabetes 5 to 10 years before it will occur clinically. Other metabolic markers are homocysteine and metalloproteinases. There are newer tests to measure insulin resistance.
Oxidized LDLc is the only marker that is linked to diabetic retinopathy. Another marker, resistin is an independent marker for obesity-related cancer, cardiovascular disease and overall mortality. A triglyceride glucose-waist circumference index has been found to be the best predictor for future development of diabetes.
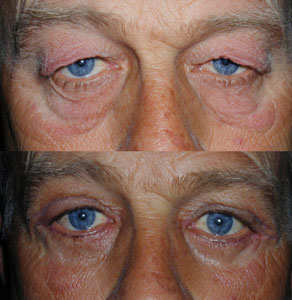
Body composition analysis
The patient measures his/her own waist circumference and body weight on body composition scales. This gives additional information about fat and muscle composition. Dr. Cadegiani’s team likes to understand what is really going on in terms of what triggers fat excess.
Questions are: what is the level of emotional overeating? How much anxiety is there in the patient’s life that leads to overeating? What is the social and cultural environment? What were previous weight loss attempts? And what is the family history in term of excessive weight?
Other important factors are to check for binge eating disorders or night eating syndrome. In addition any patient planning to go for weight loss therapy should be checked for depression, mood disorders and suicide potential.
Otherwise body composition scales by electrical bioimpedance were found to be very useful in assessing fat and muscle percentage as well as visceral fat percentage.
Aggressive clinical approach improves metabolism
Dr. Cadegiani and his group have published their own research paper in February 2017 showing that an aggressive clinical approach can prevent the need for bariatric surgery. This publication describes that in a group of 43 subjects who were thought to be bariatric surgery candidates only 3 patients (7%) went on to have the procedure done. 93% of the subjects were able to shed pounds with the method offered and avoided bariatric surgery.
They documented that clinical parameters and blood tests all improved on their program. The researchers focused on triggers that caused obesity in their patients. The measured markers were oxidized LDL cholesterol, triglycerides, the liver enzymes ALT and μGT, fasting glucose, Hemoglobin A1C, uric acid and CRP. All of these parameters improved with the modification in food intake. 81.2% of the weight loss was from the reduction of fat mass. 46.5% of patients had a normal waist circumference measurement at the end of the trial. They also achieved normal body fat and visceral fat percentages. As already stated 93% of all the patients in this trial avoided weight loss surgery, called bariatric surgery.
Dr. Cadegiani suggested that obesity should be approached with a scientifically based and responsible method. This will change the way we manage obesity.
Conclusion
Attention to detail of the patient with weight problems will allow the patient to reduce fat percentage. Waist measurements should be regularly performed as well as body composition scales measurements. This way the physician can follow the fat and muscle percentages. Key to success is to reduce the refined carb contents of food intake (sugar and starchy foods) and have a calorie deficit diet. Exercise is also an important component. An aggressive clinical approach to obesity can improve the clinical outcome and can prevent bariatric surgery.