In my 40’s when I was practicing medicine, I was dreaming about writing a medical book. This was in the mid 1980’s and I was busy seeing 30 to 40 patients a day. I would never have found the time to write a medical book at that time. I thought, perhaps I could show how patients could stay younger for longer by adopting the right life style in order to stay well. Fast forward 3 decades, and the medical book writing began. But instead of one book the project turned into 4 books. There were too many topics to cover to fit them all in one book.
Prior to writing a medical book
First of all, in 2002 I published a large website. Its structure is like a book on the Internet: Net Health Book . It contains descriptions of the major diseases, mental and physical, and their current treatment modalities. I still maintain this work. Furthermore, I started another website in 2003, a weekly blog, called “Ask Dr. Ray” . This is a compilation of interesting research. Some medical research papers can get too scientific. For this reason I translated it into easier language. The topics tend to be anti-aging topics. This blog comes out Saturdays.
Retirement hobby
When I retired in 2010 I revamped my websites. In the process the web developer suggested I should add to Net Health Book a blog (nethealthbook.com/news) where I review current health news that I find interesting. This is a weekly blog, which I publish on Wednesdays. All of this is still going on, and it gave me lots of opportunities to write and publish on a smaller scale. In addition, I finally started publishing books.
A Survivor’s Guide To Successful Aging
My first book came out with Amazon in 2014. I had joined the A4M (American Academy of Anti-Aging Medicine) in the early 2000’s. The lectures at their conferences were very open-minded and pointed out details of what one could do to delay aging and avoid premature deaths. My own experience with changing our diet in 2001, starting bioidentical hormone replacement and changing my lifestyle became topics that were part of this book. I dedicated this book “to those who are willing to work on prevention in order to achieve a longer life without disabilities”. This is still the basis of prolonging your life.
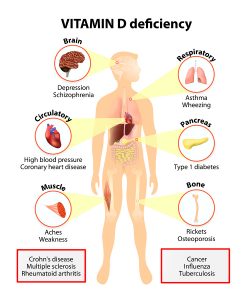
Lifestyles can be deleterious
I start out in this book describing the obesity wave and how this changes the metabolism (metabolic syndrome). I used statistics from the Framingham Heart Study to show the detrimental effects of various lifestyles on mortality. Subsequent chapters deal with food, exercise, stress and missing hormones as life-shortening factors. There is a separate chapter on vitamins and supplements. They as a group can create 5.1% longer telomeres, which translated into 9.8 years of longer life expectancy (see also a study by Dr. Xu in the book). Subsequently it describes how a change of your lifestyle can have a positive impact. Changing your eating habits and exercise activity will make a tremendous positive difference on the long term.
Successful Aging in the Kitchen
The book ends with an appendix, written by my wife: “Successful Aging in the Kitchen”. You are presented with recipes for 7 breakfasts, 7 lunches and 7 dinners. In addition she has provided 7 healthy desserts for you. Bon Appétit!
Healing Gone Wrong, Healing Done Right
In another book, which got appeared in 2016 I gave a few examples of how famous people were failed by medicine. It started already in the past: Ludwig van Beethoven’s physicians did harm instead of healing their patient. However, this is happening now as well: physicians mismanaged the health care of Elvis Presley, Churchill, Michael Jackson and JF Kennedy. The physicians treated symptoms, but they never properly attended to the causes of the ailments of their patients. The end result was premature death in all of them. Churchill who had good genetics made it to age 90, but during his last 15 years he suffered of severe disabilities.
Treatment of symptoms will fail, treatment of causes succeed
These examples of famous people’s health problems resemble to what happens to today’s patients in various office settings. Their symptoms are mostly being treated, but their causes often not. Simply treating symptoms will not work on the long term. It did not work in the past, and it does not work now.
Other chapters in this book
Other chapters in this book deal with preventing disease, keeping a healthy brain and keeping a healthy heart. Next I discuss why food matters, followed by the health of limbs and joints. Subsequently I am discussing how to keep toxins out. The next chapter deals with how to reduce the impact of cancer. It is always important to diagnose cancer as early as possible as removal by surgery has the highest success rate at an early cancer stage. The next chapter is entitled: “Stable hormones key to health”. If any of your hormones are missing (particularly around the age of menopause and/or andropause) it is time for nature identical hormone replacement. The next chapter gives you general thoughts on anti-aging. This is followed by “supplements yes, but do not overdo it”.
Alternative treatment for ADHD
A final chapter gives you an example of an alternative treatment for ADHD, where the idea of not just treating symptomatically, but treating causes is included. References and an index are also provided for the book.
Prostate Cancer Unmasked
Furthermore, I did not intend to write this book. But in early 2016 my PSA (prostate specific antigen) level jumped from 3 to 8.6. For years it had been in the 1.5 areas, then slowly increased to 3. But 8.6 was too high for comfort! I had an MRI scan done, which showed one lesion in my left prostate, which was suspicious for prostate cancer. I was referred to a urologist at the Vancouver Prostate Centre, one of the top clinics in Canada. But I had already researched the literature and came across research by Dr. Gary Onik from Ft. Lauderdale who warned me about the pitfalls of “standard therapy”.
The conservative urologist in Vancouver
The urologist in Vancouver told me that without a positive biopsy he cannot accept that the shadow on my MRI scan would be prostate cancer. And the only way they do a prostate biopsy was by random trans-rectal biopsies. He also wanted to include me in a random clinical trial where they would compare active intervention with active surveillance. I politely declined the trans-rectal prostate biopsy and the inclusion into a trial.
Assessment by Dr. Onik
I booked a flight to see Dr. Onik in Ft. Lauderdale. His method is well researched and orchestrated.
Initial assessment
He assesses you with a rectal ultrasound and he sees the prostate on a TV screen. He said right away that I had three separate lesions, one in the left as shown on the MRI scan and two in the right lobe, which was missed by the MRI scan. False negative lesions are common on MRI scans, which can become a source of cancer recurrence.
3-dimensional prostate biopsy
The following day he booked me for a 3-dimensional prostate biopsy via the perineal approach. The perineum is easy to sterilize, so there is no risk of septicemia. A metal grid with holes for biopsy needles was used to get 96 biopsies of my enlarged prostate. For a normal size prostate, Dr. Onik said about 60 biopsy needles are normal. You don’t feel anything, because you are asleep.
Cryoablation prostate surgery
Next was the cryoablation surgery of the 3 prostate cancer lesions. This happened one month after the biopsy. I was seen at the hospital in Ft. Lauderdale. The same grid from the biopsy was used to relocate exactly where the cancer lesions were. The pathologist had confirmed them as Gleason 6 and 7 prostate cancers. This was treated with Argon sounds and frozen twice. I felt nothing, because I was under a general anesthetic. But Dr. Onik told me that everything went very well. Some cancer was too close to the neurovascular bundle, so he used the NanoKnife, an invention where nano-size holes get blasted into cancer cells, but it leaves normal tissue intact.
I needed to do self-catheterization for about one month to empty my bladder, as there was a lot of swelling from the prostate hypertrophy and the surgery. But eventually my normal water works returned.
Follow-up blood work
My follow-up PSA blood work 3 months after the surgery was down to 1.0. Prior to the surgery the Oncoblot test was positive for prostate cancer. A repeat Oncoblot test 3 months after the surgery was now negative for prostate cancer. I realize that not every physician accepts this new cancer-screening test, but I felt a lot better to know that all the cancer markers were now gone.
9 cancer treatments reviewed
In my book I described a total of 9 prostate cancer treatments and their 10-year survival statistics. None of the other treatment methods were as good as Dr. Onik’s statistics. I believe it is linked to the precision of the 3-dimensional biopsy and the surgery being done through the same grid. If you do not perform the surgery this way, you miss cancer lesions and this becomes the source of failure 10 years down the road. My book details all these alternative treatments. It also has a section on lifestyle modifying factors. I needed to write this book as a service to any man who suddenly is faced with a possible diagnosis of prostate cancer.
Unmasking prostate cancer
Like me he needs to unmask the cancer. Is it really there? How far advanced is it? Which way to safely biopsy it (definitely NOT through the rectum for fear of blood poisoning=septicemia)? What is the best method to remove it? I came to the conclusion that Dr. Onik’s method was best for me. But with the information in this book you can decide what is best for you.
Medical Questions Answered
Finally I wrote my 4th book. From more than 4400 medical questions that I have answered on the site Quora.com I selected the most popular questions for this book. The editorial board of Quora said that I own the publishing rights for my answers. The questions were rephrased without changing the meaning. I selected more than 120 questions under 44 different headings.
Here are some of the areas that are covered: Acne, the best home remedies. Aging: can it be reversed? What is the limit for a human? Alcohol: how does it affect your body? Alzheimer’s disease: which foods promote brain health? Arthritis: what can you do about osteoarthritis? Back pain: what can I do about it? Cancer: why can cancer still not be cured? There are as well 15 other answers about cancer. Depression: will my depression ever go away? Diabetes: will a 600-calorie diet help diabetes control?
Further topics discussed
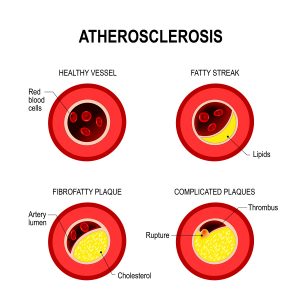
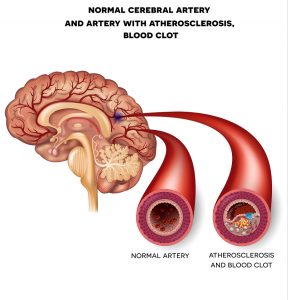
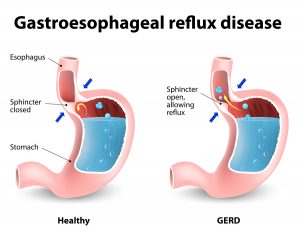
Diet: I want to get rid of sugar in my diet. How can I do this long-term? Other answers about diet are included. Exercise: How useful is cardiovascular exercise? Gut disease: Is “gluten free” food healthy? Heart disease: What can I do to clean out my arteries and reduce my risk for heart disease? Hormones: Is estrogen present in the male body? Life Expectancy: What is the theoretical life expectancy of humans? Lifestyle Habits: Can good habits change your life completely? Pain: Pain relief for a headache or other pain: Aleve, Advil or Tylenol? Pregnancy: Best age for a successful pregnancy? Prostate Cancer: How dangerous is prostate cancer? Does it kill you? Schizophrenia: What complementary approach may help a patient with schizophrenia? Sleep: What happens when you go to bed late every night? And many other answers under this topic.
And the book finishes with these topics
Sugar: will I be OK living without sugar? Vaccinations: Is there a connection between vaccinations and autism? Vitamins and supplements: Are taking vitamins and supplements healthy or are they harmful? Weight loss: I am working out every day, but I am not loosing weight. What should I do? There are many more answers under this topic. Younger for longer: What are three things I can do every day to stay younger for longer?
These are only a few selections of all of the topics dealt with in this book.
Conclusion
I have reviewed briefly why I published the books mentioned above. My prostate cancer book developed out of the necessity that I had to deal with my newly diagnosed prostate cancer in 2016. I felt that the review process I went through would be good for those men who have to face a similar situation. The anti-aging book comes from my interest in anti-aging medicine. “Healing Gone Wrong, Healing Done Right” developed from the observation that physicians in the past and often even now tend to only treat symptoms. But if a cause can be found, this should be treated, as this often leads to a permanent cure.
Treating symptoms only will not improve the patient’s condition
Treating symptoms only will not improve the patient’s condition. “Medical Questions Answered” is a collection of medical topics where I answered various medical questions. It was a way for me to cover a vast array of medical topics. Some of the topics are dealt with in depth (acne for instance); others are very short. I have also two medical blogs that come out on Wednesdays and Saturdays. I hope that some of that medical information will be useful to you.