An article in The New England Journal of Medicine stated that cardiovascular risk markers predict heart attacks and strokes. A summary of this study was also published by NBC News.
30-year follow-up of the Women’s Health Study
This is based on a 30-year follow-up study of the Women’s Health Study. In the beginning of the study all women had blood tests taken. In the beginning none of the women had cardiovascular disease. The blood tests were LDL cholesterol, lipoprotein(a) and high-sensitivity C-reactive protein (CRP). When either of these markers was high at the beginning of the clinical trial, it turns out that 30 years later the person either was dead from cardiovascular disease or had a heart attack or stroke.
More details of the study
In the beginning of the study 27,939 initially healthy U.S. women had 3 of the mentioned blood tests taken. If only one of them was elevated, there was a risk in the next 30 years to get a myocardial infarction, coronary revascularization, stroke, or death from cardiovascular causes. The initial age of the patients was 54.7 years. During the next 30 years of follow-up 3662 cardiovascular events took place. Hazard ratios for the primary end point in a comparison of the top with the bottom quintile were calculated. The following hazard ratios were derived:
- 70-fold for high-sensitivity CRP
- 36 for LDL cholesterol
- 33 for lipoprotein(a)
Each biomarker showed an independent contribution to the overall risk. The risk of developing cardiovascular disease was highest when all three biomarkers were elevated.
Traditional risk calculation
Cardiologists calculated risk for cardiovascular events by the traditional 10-year estimates of risk. The authors suggest that physicians should do screening blood tests with these three biomarkers. If any of the biomarkers is elevated, measures to reduce cardiovascular risk should be initiated. This will be very effective to prevent cardiovascular events for the next 30 years.
Be proactive, prevent heart disease
As we get older, many people develop elevations of high-sensitivity CRP, LDL cholesterol and lipoprotein (a). But don’t wait for this to happen. Here are 9 steps you can follow to prevent it.
- Maintain a healthy weight
- Quit smoking
- Choose good nutrition
- Be physically active
- Treat hypertension adequately
- Manage diabetes, if you have it
- Stress management
- Limit alcohol intake
- Get enough sleep
Comments to the steps you can take to prevent cardiovascular disease
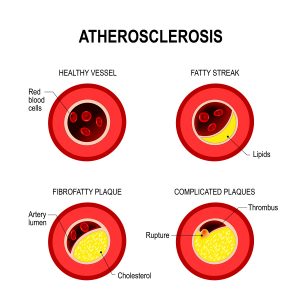
The ideal body mass index is between 21.0 and 22.0. I found that the fasting mimicking diet helps me to stay in that BMI range. Good nutrition eliminates red meat and emphasizes vegetables and salads. Fish, lean chicken and turkey meat are healthy. Avoid all processed meats like sausages. Watch your calorie intake to keep your body mass index stable. In addition, avoid excessive salt and sugar intake. Avoid highly processed carbohydrates and processed food. Eliminate fried fast food, chips and baked goods from your diet as they contain trans fats. Trans fats cause hardening of the arteries.
Aim to get 30 to 60 minutes of daily activity. Do two or more strength training sessions a week. This raises the protective HDL cholesterol and prevents cardiovascular disease. Excessive alcohol intake leads to cardiovascular disease and high blood pressure. Limit your alcohol intake, if you find it hard to eliminate it altogether.
Conclusion
A unique 30-year follow-up study of the Women’s Health Study identified three risk factors that a doctor can be determin from a blood sample. They predict whether a person will develop cardiovascular disease 30 years down the road. The three risk factors are high-sensitivity CRP, LDL cholesterol and lipoprotein (a). The best approach to prevention of heart disease is to adopt the approach of the Mayo Clinic described above. It comes down to the basics of good nutrition, regular exercise, maintaining a healthy weight, limiting excessive alcohol intake and stress management.